Research Article, J Nephrol Ren Dis Vol: 1 Issue: 2
Assessment of Fibroblast Growth Factor-23 ( Fgf23) as Risk Factor for Diastolic Dysfunction in Hemodialysis Patients
Malihe Mohammad Hosseini1, Narges Sadat Zahed2*, Muhanna Kazempour2, Roxana sadeghi3, Seyed Morvarid Dadras3 and Samira Tabiban4
1Department of Nephrology, Shahid Beheshti University of Medical Science, Tehran, Iran
2Department of Internal Medicine, Shahid Beheshti University of Medical Science Tehran, Iran
3Department of Cardiovascular Diseases, Shahid Beheshti University of Medical Science, Tehran, Iran
4Rajaie cardiovascular Medical and research Center, Iran University of Medical Science, Tehran, Iran
*Corresponding Author : Narges Sadat Zahed
Department of Internal medicine, Division of Nephrology, Loghman Hakim Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Tel: +982151025000
Fax: +982122439784
E-mail: lcrdc.sbum@gmail.com
Received: February 16, 2017 Accepted: February 18, 2017 Published: February 26, 2017
Citation: Hosseini MM, Zahed NS, Kazempour M, Sadeghi R, Dadras SM, et al. (2017) Assessment of Fibroblast Growth Factor-23 ( Fgf23) as Risk Factor for Diastolic Dysfunction in Hemodialysis Patients. J Nephrol Ren Dis 1:2.
Abstract
Background: Cardiovascular disease is the most common cause of death in patients with chronic kidney disease. Diastolic dysfunction is an important risk factor result in development of advanced cardiovascular disease. Fibroblast growth factor- 23 (FGF23) secretes in response to hypophosphatemia as a result of renal excretion of phosphate. Elevation of serum FGF23 is one of the possible causes of diastolic dysfunction. The aim of the current study was to investigate association between Serum levels of FGF23 and diastolic dysfunction in hemo dialysis patients.
Methods: 100 hemodialysis patients were enrolled in the study between October 2015 and February 2016. Cardiac diastolic function was assessed by tissue Doppler imaging and ejection fraction>50% considered to be investigated. Serum FGF23, cholesterol, triglyceride, fasting blood sugar, 25(OH)vitD3, Phosphorus, calcium, alkaline phosphatase, PTH and hemoglobin were measured in all patients. Statistical analysis preformed using SPSS version 16(Chicago, USA).
Results: FGF 23 was elevated in 69% (52/75) of patient and had correlation with serum levels of phosphor and PTH, while Serum levels of FGF23 was not significantly difference between patients whit diastolic dysfunction versus other cardiac problem (p=0.158).
Conclusions: After elimination of secondary causes of diastolic dysfunction, no association was found between serum FGF23 levels and diastolic dysfunction among hemodialysis patients.
Keywords: Hemodialysis; Diastolic dysfunction; FGF23
Introduction
Chronic renal failure (CRF) increased risk of cardiovascular disease (CVD) and mortality. Two categories of traditional or classic risk factors and elements associated with renal failure or non-classical risk factors are considered as underlying causes of CVD. recognition and control of traditional factors such as hypertension, diabetes and dyslipidemia, had little impact on the prognosis of cardiovascular disease among CRF patients, whereas diagnosis and management of non-classical risk factors like anemia, hyperphosphatemia, increased serum levels of Fibroblast growth factor-23 (FGF23), vitamin D deficiency, hyperparathyroidism and systemic inflammation has been far better impact on prognosis of cardiovascular disease [1-3]. FGF23 Secretion is in response to hyperphosphatemia and lead to renal excretion of phosphate [4]. FGF23 increasing, occurs before elevation of serum phosphorus and PTH level in CRF patients [5]. Increased serum levels of FGF23 are associated with impaired vascular function, vascular calcification and left ventricular hypertrophy. Elevated FGF23 levels are demonstrated as possible causes of diastolic dysfunction [6,7]. Diastolic dysfunction is risk factor of development and progression of advanced cardiovascular disease. Therefore, FGF23 increasing is associated with cardiovascular complications and increased mortality among chronic renal failure [8].
Christian Faul et al. noted that Elevation of serum FGF23 is associated with progression of kidney failure and increased mortality rate. They also illustrated increased FGF23 as strong risk factor for cardiovascular disease among patients with CRF [6]. We are aware of the high incidence of diastolic dysfunction among CRF patients as reported by Farshid et al. diastolic heart function, is an important factor leading mortality of patients with renal failure [9]. A literature by Bleskestad et al. reported if patients with renal impairment first treated with calcitriol and then with sevelamer, reduction in serum levels of FGF-23 is produced previous findings considered management of high FGF23 levels by reducing phosphorus levels. Finally it is not entirely clear if FGF23 levels reduction result in better diastole function or prevent diastolic dysfunction [10].
Dogan et al. noted that Significant relationship between the indices Diastolic function as E′ and IVRT, with levels of FGF23 is exist among type 1 diabetes with early stages of diabetic nephropathy, whereas similar relationship does not find in type 1 diabetic patients without nephropathy, as well as in healthy individual [11] so the role of FGF23 in diastolic dysfunction may be stronger in end stages of renal disease. By review of previous studies the effect of elevated FGF23 serum levels on diastolic dysfunction among hemodialysis patients is not clear. Aim of the current study was to investigate the relationship between FGF23 levels and diastolic dysfunction in dialysis patients.
Methods
Subjects
This descriptive study was performed on 100 hemodialysis patients of Loghman Hakim Hospital and Ashrafi Esfehani Hospital were enrolled in the study between octobre 2015 and February 2016. Written consent was obtained from all patients and the study protocol was approved by ethical committee of Shahid Beshti university of medical sciences (protocol no: 571). Exclusion criteria was hemodialysis<3month, age<18 years, anemia (hemoglobin<10), uncontrolled hypertension, history of heart disease; (EF less than 50%, heart surgery, vascular stent, CABG, arrhythmia, severe valvular disease) and inadequacy of dialysis (KT/V<1.2) serum levels of FGF 23, cholesterol, triglyceride, fasting blod sugar, 25(OH)vitD3, phosphorus, calcium, alkaline phosphatase, PTH and hemoglobin were measured and echo cardio graphic parameters was determine among all included subjects.
Biochemical parameter
Blood sample were taken from all patients after 12 hours of fasting and stored at -80â�?¦C until analysis. typical laboratory methods were used to assess fasting blood sugar (FBS), phosphorus (P), calcium (Ca), alkaline phosphatase (alk-p) parathyroid hormone (PTH),25 (OH)vit D3, c-reactive protein (CRP)and hemoglobin. measurement of fibroblast growth factor-23 (FGF23)serum plasma levels performed by ELISA kit according to manufacture ‘s instruction. The lower limit of detection (LLD) of this assay was defined as the lowest detectable concentration that could be differentiated from zero. The detectable range described as 15.6-100 pg/mL. Normal range of FGF-23 plasma levels was reported as 31.3 ± 8.4 pg/dL by studying healthy population [12].
Echocardiographic assessment
Doppler Tissu Imaging (DTI) (Phillips Epiqe 7c) was performed to assess cardiac function during non-dialysis day for patients who had just Diastolic dysfunction with preserved systolic function (without any other cardiac problem). Measurements of quantitative data such as the left ventricular end diastolic (LVED) volume, mitral annular velocity (E′), late diastolic annular velocity (A′), mitral valve fellow to mitral annular motion index (E/E′) isovolomic relaxtion time (IVRT), iso volomic contraction time (IVCT), deceleration time of early diastolic mitral flow (Dec T), propagation velocity (PV), systolic fellow in pulmonary venous (S), D duration ADure were done (Table 3).
Statistical analyses
All values were expressed as mean ± (standard deviation) SD. Quantitative data was analyzed using student T- test and Mann- Whitney test, while chi-square test was used to analyze qualitative variables. Pearson rho correlation was used for normally distributed variables and spearman’s rho correlation was performed to assess the correlation of non-normally distribute data.
All tests were done two-sided, and P<0.05 was considered statistically significant data analysis performed by SPSS statistics version 16.0 (Chicago, USA).
Results
Among (75/100) hemodialysis patients (50 men) 52% (39/75) of patients had diastolic dysfunction with preserved systolic function (without other cardiac problem) and (36/75) 48% patient had other cardiac problem. Demographic characteristics of patients are presented in Table 1. The mean age of patients with diastolic dysfunction (53 ± 13/63) were lower than other cardiac problem (61/36 ± 12/6) (p=0/007). Laboratory and echocardiographic data are presented in Table 2.
| Variables | Total | Diastolic dysfunction | Other cardiac problem | P value |
|---|---|---|---|---|
| Women/Men (n) | 25F/50M | 14F/25M | 11F/25M | 0/807 |
| Age( years) | 57/1 ± 13/7 | 53 ± 13/63 | 61/36 ± 12/6 | 0/007 |
| Dialysis sufficiency (%) | 66 | 35 (89/7) | 31(86/1) | 0/73 |
| Over weight before dialysis (<2)kg | 36 | 15(38/5) | 21(58/3) | 0/108 |
| Past history | ||||
| Diabetes (%) | 35 | 15(38/5) | 20(55/6) | 0/168 |
| Dyslipidemia (%) | 5 | 3 (7/7) | 2(5/6) | 1 |
| Cardiovascular disease | ||||
| Ischemic heart disease (%) | 14 | 6 (15/4 ) | 8(22/2) | 0/557 |
| Hypertension (%) | 48 | 23(59) | 25(69/4) | 0/471 |
| Smoking (%) | 7 | 3 (7/7) | 4 (11/1) | 0/704 |
| Opium (%) | 7 | 4 (10/3) | 3(8/3) | 1 |
| Alcohol (%) | 1 | 0 (O) | 1(2/8) | 0/480M |
| Medication | ||||
| ACE inhibitor, n (%) | 6 | 3 (7/7) | 3 (8/3) | 1 |
| ARB, n (%) | 11 | 7(17/9) | 4 (11/1) | 0/52 |
| Beta blockers, n (%) | 20 | 13 (33/3 ) | 7 (19/4) | 0/201 |
| Calcium channel blockers (%) | 23 | 12 (30/8) | 11 (30/6) | 1 |
| Diuretics (%) | 9 | 4 (10/3) | 5 (13/9) | 0/73 |
| Statin (%) | 13 | 6 (15/4) | 7 (19/4) | 0/763 |
| Fibrate (%) | 2 | 2 (5/1) | 0(0) | 0/494 |
Table 1: Demographic and laboratory data of patients.
| Variables | Total | Diastolic dysfunction | Other cardiac problem | P value |
|---|---|---|---|---|
| 25(OH) vitaminD | 30/1 ± 17/3 | 29/68 ± 15/75 | 30/62 ± 19/17 | 0/82 |
| Hemoglobin,g/dL | 11/04 ± 1/35 | 11/16 ± 1/29 | 10/92 ± 1/42 | 0/437 |
| Cholesterol (mg/dL) | 133/2 ± 33 | 131/4 ± 29/09 | 135/2 ± 37/06 | 0/623 |
| Triglyceride (mg/dL) | 128/5 ± 76/2 | 135 ± 68/7 | 121/5 ± 84/0008 | 0/450 |
| HDL (mg/dL) | 37/6 ± 9/2 | 36/9 ± 9/5 | 38/3 ± 8/80 | 0/533 |
| LDL (mg/dL) | 71/3 ± 21/6 | 71/22 ± 22/5 | 71/3 ± 20/9 | 0/991 |
| Phosphorus (mg/dL) | 5/2 ± 1/5 | 5/17 ± 1/25 | 5/15 ± 1/67 | 0/937 |
| Calcium (mg/dL) | 8/9 ± 351/03 | 8/89 ± 0/89 | 8/9o ± 1/17 | 0/956 |
| ALP | 299 ± 146/2 | 319/44 ± 148/73 | 267/52 ± 142/01 | 0/206 |
| FBS | 127/2 ± 67 | 116/92 ± 57/98 | 138/30 ± 74/78 | 0/047 |
| Hs-CRP | 7/5 ± 4/8 | 6/131 ± 6/55 | 9/0024 ± 11/2 | 0/561 |
| PTH | 159/9 ± 145/9 | 180/38 ± 155/34 | 136/35 ± 132/67 | 0/266 |
| FGF23(pg/Dl) | 461/3 ± 351/03 | 533/587 ± 365/92 | 382/96 ± 320/99 | 0/158 |
Table 2: Comparison between laboratory data of patients with and without diastolic dysfunction.
| Variables | Normal Range | Maximum | Minimum | ST. deviation | Mean |
|---|---|---|---|---|---|
| LVE diastolic dysfunction | Female 2/8-8/9: Male 2/9-4/ 5: | 2 | 4/83 | 0/52 | 4/7 |
| E’ | 12 - 5 | 11 | 4 | 1/9 | 2/6 |
| A’ | 12 - 8 | 9 | 2/4 | 1/8 | 7/5 |
| S | 110 - 5 | 15 | 7/5 | 1/8 | 9/4 |
| E | 36 ± 16 | 113 | 42 | 17/2 | 70 |
| A | 26 ± 13 | 150 | 20 | 13/2 | 76/3 |
| VP | <20 | 67 | 20 | 2 | 27/1 |
| Deceleration time(msec) | 240 - 160 | 815 | 93 | 29/3 | 126/2 |
| IVRT | 90 - 70 | 109 | 40 | 17/5 | 35/6 |
| IVCT(mm) | >60 | 105 | 82 | 13/6 | 32/1 |
| E/E’ | 18/88-4/65 | 58/6 | 2/9 | 2/1 | 18/8 |
| PAP | 42 - 30 | 80 | 52 | 1/2 | 52/6 |
| ADure | 180 - 122 | 32 | 80 | 13/1 | 23 |
| Ps | 4 - 8 | 62 | 52 | 10/3 | 49/4 |
| Pd | 6 - 3 | 28 | 56 | 7/8 | 82 |
| EF | <20 | 22 | 50 | 11/02 | 47 |
Table 3: Echocardiographic data of patient with diastolic dysfunction.
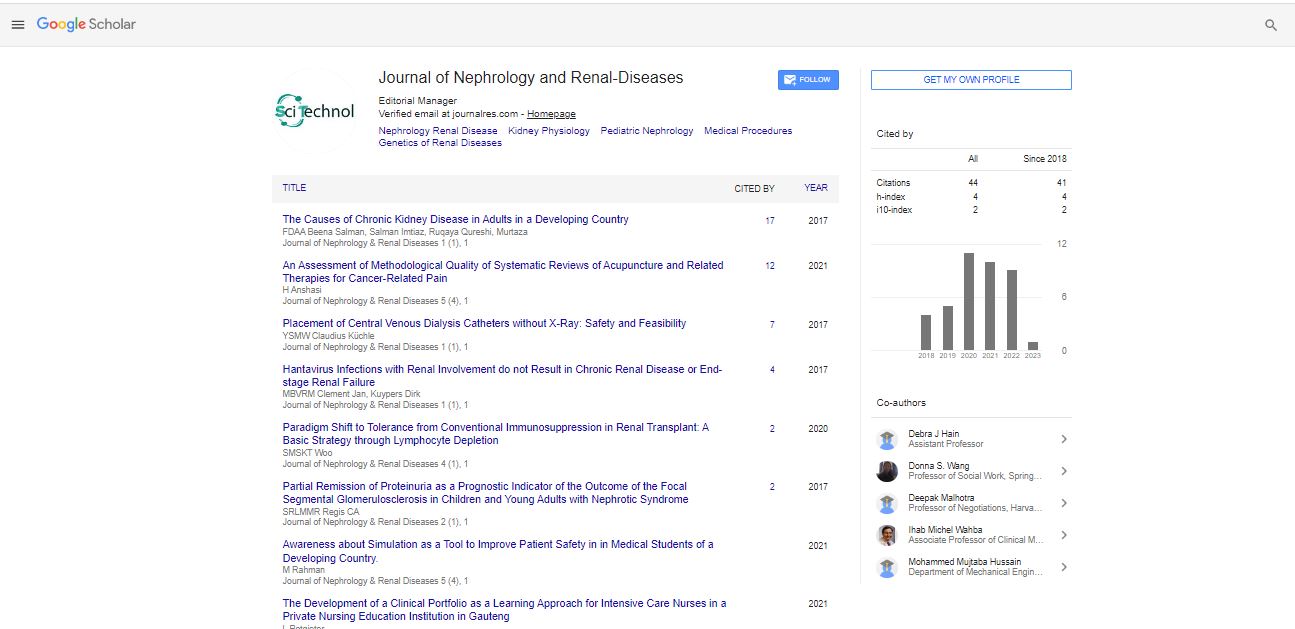
FGF23 was elevated in 69% (52/75) of patient and had correlation with serum levels of phosphor and PTH, while serum levels of FGF 23 was not significantly difference between patients whit diastolic dysfunction versus other cardiac problem (p=0.158) (Figure 1). Demographic and laboratory data between two groups was not significantly difference but fasting blood sugar (116/92 ± 57/98) among patients with diastolic dysfunction was lower than nondiastolic dysfunction (138/30 ± 74/78) (p=47/70) (Figure 2).
Discussion
The most common cause of death in dialysis patients is cardiovascular events [9].
Diastolic dysfunction is an independent factor for cardiovascular events among hemodialysis patients with preserved systolic function [13]. Prashant et al. reported CKD is associated with moderate to severe diastolic dysfunction and left ventricular diastolic dysfunction has been observed even in the early stages of CKD [14]. Maizel et al. concluded that sevelamer (as phosphate binder) not only reduces serum phosphate and FGF23 levels but also decrease diastolic dysfunction [15].
Some studies found statistically significant relation between serum FGF23 levels and diastolic dysfunction [11,15,16], but others could not confirmed the correlation. In our study, patients’ sex was not statistically significant difference between two groups, but subjects with diastolic dysfunction were younger. This fi!nding was against the Okamoto study, which reported female more than male had diastolic dysfunction, and patients with diastolic dysfunction was older than patient with non-diastolic dysfunction problems. Otherwise Okamato’ patients were not on hemodialysis and he was not excluding valvular heart disease. We found no association between serum FGF23 levels and diastolic dysfunction in dialysis patients after elimination of secondary causes. Our results are in agree with previous studies that concluded FGF23levels, was not significantly in associate with diastolic dysfunction [17].
We found that in younger dialysis patient diastolic dysfunction was first manifestation in echocardiography and there was no correlation between serum levels of FGF23 and diastolic dysfunction, because we exclude patient with other cardiac problem.
Review of mentioned articles shows that there is no consensus on the relationship between serum FGF-23 level and diastolic dysfunction in dialysis patients. Further studies are needed to verify these findings. Sakane et al. concluded that patients with preserved left ventricular function and no-CKD, patients with elevated FGF23 concentrations were at higher risk for diastolic dysfunction [16].
Dogan et al. noted that there was Significant relationship between diastolic function as E′ and IVRT, with serum levels of FGF-23 in type 1 diabetes with early stages of diabetic nephropathy [11], which this relationship does not exist in type 1 diabetic patients without nephropathy, as well as in healthy individuals. They surveyed young adult type 1 diabetic patients with GFR>60 ml/min, but we surveyed diastolic dysfunction in dialysis patients. This may account for the difference in results between the current study and their results. Sharon et al. reported that Cinacalcet significantly reduced the serum levels of FGF-23 in CKD and treatment-induced reductions in serum FGF23, reduce mortality and cardiovascular events in CKD [18] Maizel et al. surveyed mice with CRF and concluded FGF23 serum level was not reduced by sevelamer. Serum phosphate was independently correlated with LV diastolic function, but not FGF23. So, sevelamer first improved diastolic dysfunction and secondarily prevented LVH [15].
Conclusions
After elimination of secondary causes of diastolic dysfunction, no association was found between serum FGF23 levels and diastolic dysfunction in dialysis patients.
Acknowledgment
The authors would like to thank the clinical research development center (CRDC) of Longman Hakim Hospital, Shahid Beheshti University of medical science, Tehran, Iran for their support, cooperation and assistance throughout the period of study.
References
- Dobnig H, Pilz S, Scharnagl H, Renner W, Seelhorst U, et al. (2008) Independent association of low serum 25-hydroxyvitamin D and 1, 25-dihydroxyvitamin D levels with all-cause and cardiovascular mortality. Arch Intern Med 168: 1340-1349.
- Akin F, Ayça B, Köse N, Celik O, Yilmaz Y, et al. (2014) Serum vitamin D and c-reactive protein levels are independently associated with diastolic dysfunction. J Investig Med 62: 43-48.
- Ku Y-C, Liu ME, Ku CS, Liu TY, Lin SL (2013) Relationship between vitamin D deficiency and cardiovascular disease. World J Cardiol 5: 337-346.
- Westerberg PA, Linde T, Wikström B, Ljunggren O, Stridsberg M, et al. (2007) Regulation of fibroblast growth factor-23 in chronic kidney disease. Nephrol Dial Transplant 22: 3202-3207.
- Isakova T, Wahl P, Vargas GS, Gutiérrez OM, Scialla J, et al. (2011) Fibroblast growth factor 23 is elevated before parathyroid hormone and phosphate in chronic kidney disease. Kidney Int 79: 1370-1378.
- Faul C (2012) Fibroblast growth factor 23 and the heart. Curr Opin Nephrol Hypertens 21: 369-375.
- Pilz S, Tomaschitz A, März W, Drechsler C, Ritz E, et al. (2011) Vitamin D, cardiovascular disease and mortality. Clin Endocrinol (Oxf) 75: 575-584.
- Pecoits�Filho R, Bucharles S, Barberato SH (2012) Diastolic heart failure in dialysis patients: mechanisms, diagnostic approach, and treatment. Semin Dial 25: 35-41.
- Farshid A, Pathak R, Shadbolt B, Arnolda L, Talaulikar G (2013) Diastolic function is a strong predictor of mortality in patients with chronic kidney disease. BMC Nephrol 14: 280.
- Bleskestad IH, Bergrem H, Hartmann A, Godang K, Gøransson LG (2012) Fibroblast growth factor 23 and parathyroid hormone after treatment with active vitamin D and sevelamer carbonate in patients with chronic kidney disease stage 3b, a randomized crossover trial. BMC Nephrol 13: 49.
- Dogan B, Arikan IH, Guler D, Keles N, Isbilen B, et al. (2016) Fibroblast growth factor-23 but not sKlotho levels are related to diastolic dysfunction in type 1 diabetic patients with early diabetic nephropathy. Int Urol Nephrol 48: 399-407.
- Smith ER, McMahon LP, Holt SG (2013) Method-specific differences in plasma fibroblast growth factor 23 measurement using four commercial ELISAs. Clin Chem Lab Med 51: 1971-1981.
- Han JH, Han JS, Kim EJ, Doh FM, Koo HM, et al. (2015) Diastolic dysfunction is an independent predictor of cardiovascular events in incident dialysis patients with preserved systolic function. PLoS One 10: e0118694.
- Sidmal PS, Mallikarjun H, Shekarappa K (2015) Pattern and severity of left ventricular diastolic dysfunction in early and end stage renal disease patients with or without dialysis in rural population in South India. Int J Biomed Res 6: 546-553.
- Maizel J, Six I, Dupont S, Secq E, Dehedin B, et al. (2003) Effects of sevelamer treatment on cardiovascular abnormalities in mice with chronic renal failure. Kidney Int 84: 491-500.
- Sakane K, Ohzeki M, Morita H, Hoshiga M, Ishizaka N (2004) Elevated Fibroblast Growth Factor-23 levels is Associated with Diastolic Dysfunction among No-CKD Patients with Preserved Left Ventricular Ejection Function. J Card Fail 10: S169.
- Okamoto Y, Fujita S, Morita H, Kizawa S, Ito T, et al. (2016) Association between circulating FGF23, α-Klotho, and left ventricular diastolic dysfunction among patients with preserved ejection fraction. Heart Vessels 31: 66-73.
- Moe SM, Chertow GM, Parfrey PS, Kubo Y, Block GA, et al. (2015) Cinacalcet, FGF23 and cardiovascular disease in hemodialysis: the EVOLVE trial. Circulation 132: 27-39.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi