Research Article, Int J Ment Health Psychiatry Vol: 8 Issue: 2
Anxiety and Burden among Caregivers of Onco-Hematology Patients
Latifa khelifa1*, Ines Feki2, Rym Mallekh3, Moez Mdhaffer1 and Moez Elloumi1
1Department of Hematology, University Hospital Hedi Chaker Sfax, Tunisia
2Department of Psychology, University Hospital Hedi Chaker Sfax, Tunisia
3Department of Community Medicine, University Hospital Hedi Chaker Sfax, Tunisia
*Corresponding Author :Latifa khelifa, Department of Hematology, University Hospital Hedi Chaker Sfax, Tunisia, E-mail: Khelifa.la@gmail.com
Received date: 07 December, 2021, Manuscript No. IJMHP-21-46818;
Editor assigned date: 10 December 2021, PreQC No. IJMHP-21-46818 (PQ);
Reviewed date: 27 December 2021, QC No. IJMHP-21-46818;
Revised date: 07 Februay 2022, Manuscript No. IJMHP-21-46818 (R);
Published date: 01 April 2022, DOI: 10.4172/2471-4372.1000212.
Citation: Latifa k, Ines F, Rym M, Moez M, Moez E (2022) Anxiety and Burden among Caregivers of Onco-Hematology Patients. Int J Ment Health Psychiatry 8:2. Volume 8
Abstract
The occurrence of cancer in a family member denounces the whole family. Few studies have explored anxiety and burden in parents responsible for the management of patients hospitalized with malignant hematologic pathologies. The Zarit scale and the STAI anxiety scale were deployed to study the degree of parental burden and the level of anxiety, and to investigate possible correlations between these two parameters.
Methods: Descriptive and analytical cross-sectional study over 3 months concerning parents of patients hospitalized in the hematology department at University Hospital Hedi Chaker Sfax.
Results: Our study involved 22 caregivers. In 77% of cases, these were mothers with a median age of 38 years, the level of education was high school in 50% of cases and economic level was considered middle in 73% of cases. The reported burden varied between mild to moderate and moderate to severe in 90% of cases. The analytical study demonstrated a statistically significant correlation between the level of burden and the sex of the patient, in favor of a more burden with the female sex of the patient, the duration of the disease progression and the number of hospitalizations. AT scale was in median of 30 and very low in 91% of cases. AS scale was in median of 35 and low to medium in 50% of cases. The level of anxiety studied using the STAI scale was positively associated with parent’s study level.
Conclusion: It’s an important subject not adequately treated even though it has a major impact on the results of care and the quality of life for both patients and caregivers.
Keywords: Burden, Anxiety, Psycho, Oncology, Parents, Cancer, Hematology
Introduction
Now a day, cancer could be considered as a chronic disease that impacts potentially the public health. In fact, it is the second cause of death in the world including hematologic malignancies since they are considered (especially leukemia and lymphoma) the first childhood cancer. These pathologies are sudden and aggressive requiring urgent and long treatment, leaving physical and psychological sequels. Obviously psycho oncology is an important aspect of care after those patients, so serious challenges have to be taken in account for better cancer patient’s management. Recently, the survival rate of cancer has improved thanks to supportive care and therapeutic advances. Unfortunately, this gain has been associated with an increase in the cost, length and frequency of hospitalizations and a rise in psychological problems among patients and their relatives [1]. The latter, find themselves confronted not only to their ordinary tasks but also to be an intermediary with the care team and even a main actor in the management of such serious patient. These difficulties facing the parent are considered the burden associated to the pathology. Hoening and Hamitton in 1996 describe two type of burden, an objective one related to anything that breaks the family unit and subjective category expressed by the reported feeling of burden [2].
This multidimensional burden that results from caring for a cancer patient is related to caregivers’ negotiations about their role because they may not be used to the care they must offer or may be unaware of it or not able to provide it. According to Lazarus and Folkman’s original stress and adjusted model 1984, if perceived demands exceed available resources it would be a decline in quality of life as consequences to the poor adaptation. In addition, studies focusing on the impact of cancer on the families all over the world confirm that parents experience a very high degree of psychosocial stress during the first period of diagnosis, during the treatment and even after remission [3,4]. They are more likely to suffer from generalized anxiety, depression, denial, nervousness and loss of self-esteem. According to Freud, anxiety is an unpleasant emotional state or a human condition which includes the psychological experience and the behavior. The exploration of anxiety among parents of children with chronic diseases are interesting because the evidence suggests an irrefutable correlation between the child’s illness or symptoms and his parent anxiety, leading some authors to believe that parental stress is a factor in the patient psychological disorder increasing the risk of his poor resilience. In this context, we carried out a study to measure the burden expressed by a parent accompanying a hematologic malignancy patient and to study its relationship with clinical and psychological (anxiety) parameters [5].
Materials and Methods
Population: This is a cross-sectional study concerning the parents of patients hospitalized at the department of hematology in the University Hospital Hédi Chaker Sfax for a malignant pathology during the period between December 2019 and March 2020 [6].
Exclusion criteria
- Parent not hospitalized
- Patient in serious condition (shock, DIVC, etc.)
- Short hospital stays (less than 48 hrs)
The parent is informed in the morning of the current study and his oral consent is required. The questionnaire is asked by the same person to all parents in the afternoon or evening. The answers are collected directly on the collection sheet [7].
We used: 1/Socio-demographic and clinical data collection sheet concerning the parent and the patient 2/Scales [8].
Zaria scale: The “burden” variable is measured by the Burden Inventory (BI). This is a questionnaire used in this area. This one-dimensional 22-item scale is rated from 0 to 4, depending on how much the caregiver experiences a particular negative emotion. Adding all the items together gives a total score between 0 and 88. The score indicates that the burden is light between 21 and 40, moderate between 41 and 60, and severe beyond 61. The BI makes it possible to quantify by a synthetic score, the psychological, physical, emotional and social repercussions of the burden [9,10].
STAI scale: Anxiety is measured by the State Trait Anxiety Inventory (STAI) of spielberger. This questionnaire is subdivided into two parts; state anxiety (20 items)=the feeling of apprehension and momentary tension, linked to a specific event and anxiety treated (20 items)=the stable and generalized tendency to experience a certain degree of anxiety [11].
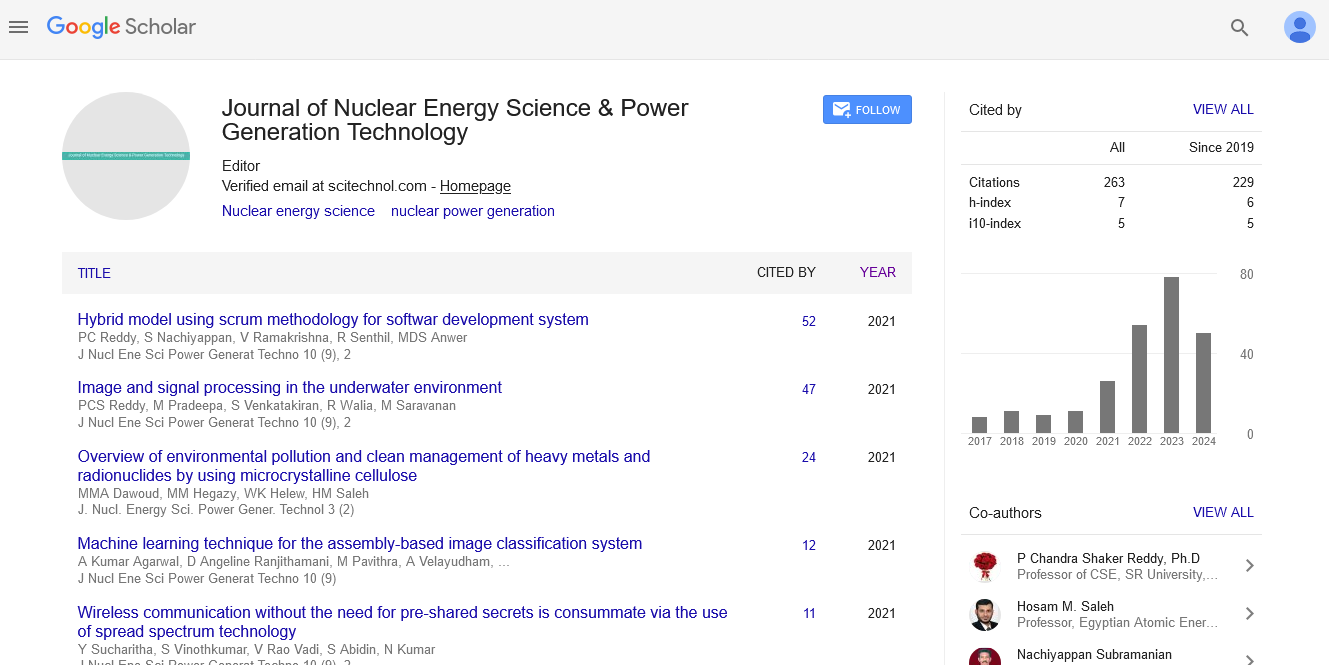
Statistics: All the data are gathered in an SPSS 20 table to allow the descriptive study. The results concerning the qualitative variables are expressed in calambres and bars. The variables of quantities are reported by their medians and extreme values (max, min). The different scales considered are expressed in histogram [12,13]. The studied sample is small N<30 as well as the distribution do not follow the normal law (Figures 1-14). So Kruskal Wallis nonparametric tests were used to look for associations between Zarit score and STAI with qualitative data and Spearman's nonparametric correlation study for quantitative variables. The p ≤ 0.05 value is considered statistically significant (Tables 1 - 3) [14].
| Parameters | Number (n) | Percentage (%) | |
|---|---|---|---|
Parents |
22 |
100 |
|
Gender |
M |
1 |
4.5 |
F |
21 |
95 |
|
Family relationship |
Mothers |
17 |
77.3 |
Spouse |
3 |
13.6 |
|
Siblings |
2 |
4.5 |
|
Age |
≤ 38 years |
10 |
45.4 |
>38 years |
11 |
50 |
|
Marital status |
Widow |
1 |
4.5 |
Single |
2 |
9.1 |
|
Married |
19 |
86.4 |
|
Study level |
Unschooled |
2 |
9.1 |
Primary or secondary |
11 |
50 |
|
Superior |
9 |
40.6 |
|
Employment |
Absent |
11 |
50 |
Occasional |
3 |
13.6 |
|
Stable |
3 |
13.6 |
|
Lost |
5 |
22.7 |
|
Salary |
Low |
5 |
22.7 |
Average |
16 |
72.7 |
|
Comfortable |
1 |
4.5 |
|
Number of children in charge |
0 |
4 |
18.1 |
≥ 1 |
18 |
81.8 |
|
Pathological history |
Absent |
16 |
72.7 |
Somatic disease |
5 |
22.7 |
|
Including psychological illness |
1 |
4.5 |
|
Patients |
22 |
100 |
|
Gender |
M |
13 |
60 |
F |
9 |
40 |
|
Age |
<18 years |
16 |
72 |
≥18 years |
5 |
22.7 |
|
Pathological history |
Present |
3 |
13.6 |
Absent |
18 |
81.8 |
|
Diagnosis |
LAL B |
12 |
54.5 |
LAL T |
3 |
13.6 |
|
LAM |
5 |
22.7 |
|
LAM 3 |
1 |
4.5 |
|
LBGC |
1 |
4.5 |
|
Current disease state |
At diagnosis |
12 |
54.5 |
In remission |
5 |
22.7 |
|
Progression or relapse |
5 |
22.7 |
|
Disease course duration |
≤ 30 days |
11 |
50 |
>30 days |
10 |
45.4 |
|
Table 1: Characteristic of the studied population.
LAL B=acute lymphoblastic leukemia B, LAL T=acute lymphoblastic leukemiaT, LAM 3=promyelocytic leukemia, LAM=acute myeloid leukemia.
| Rhodespearn | Patientae | Parents | AE | AT | Diseaseduratn | Hospitalisationnumr |
|---|---|---|---|---|---|---|
| Signification | 0,86 | 0,13 | 0,39 | 0,80 | 0,04 | 0,01 |
Table 2: Study of the correlation between Zarit scale and quantitative population characteristic’s.
| Parameters | AT | p | AE | p | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Verylow | Low | Medium | High | Very high | Verylow | Low | Medium | High | Very high | ||||
Parent Gender |
M |
1 |
0 |
0 |
0 |
0 |
0,75 |
0 |
1 |
0 |
0 |
0 |
0,48 |
F |
19 |
2 |
0 |
0 |
0 |
11 |
8 |
2 |
0 |
0 |
|||
Educational level |
Absent |
2 |
0 |
0 |
0 |
0 |
0,43 |
0 |
1 |
1 |
0 |
0 |
0,05 |
Primary or secondary |
10 |
1 |
0 |
0 |
0 |
4 |
6 |
1 |
0 |
0 |
|||
university |
8 |
1 |
0 |
0 |
0 |
7 |
2 |
0 |
0 |
0 |
|||
Parent employment |
Absent |
9 |
2 |
0 |
0 |
0 |
0,17 |
4 |
6 |
1 |
0 |
0 |
0,22 |
lost |
3 |
0 |
0 |
0 |
0 |
1 |
1 |
1 |
0 |
0 |
|||
Stable |
5 |
0 |
0 |
0 |
0 |
3 |
2 |
0 |
0 |
0 |
|||
Occasional |
3 |
0 |
0 |
0 |
0 |
3 |
0 |
0 |
0 |
0 |
|||
Life economic level |
Low |
5 |
0 |
0 |
0 |
0 |
0,55 |
2 |
2 |
1 |
0 |
0 |
0,55 |
average |
14 |
2 |
0 |
0 |
0 |
8 |
7 |
1 |
0 |
0 |
|||
confortable |
1 |
0 |
0 |
0 |
0 |
1 |
0 |
0 |
0 |
0 |
|||
Marital status |
Widow |
1 |
0 |
0 |
0 |
0 |
0,56 |
1 |
0 |
0 |
0 |
0 |
0,74 |
single |
2 |
0 |
0 |
0 |
0 |
1 |
1 |
0 |
0 |
0 |
|||
Marrid |
17 |
2 |
0 |
0 |
0 |
9 |
8 |
2 |
0 |
0 |
|||
Age |
>38 ans |
10 |
1 |
0 |
0 |
0 |
0,94 |
7 |
4 |
0 |
0 |
0 |
0,40 |
≤38 ans |
9 |
1 |
0 |
0 |
0 |
4 |
5 |
1 |
0 |
0 |
|||
Pathological history |
nothing |
15 |
1 |
0 |
0 |
0 |
0,27 |
8 |
6 |
2 |
0 |
0 |
0,61 |
≥1 |
5 |
0 |
0 |
0 |
0 |
3 |
2 |
0 |
0 |
0 |
|||
Including psychological history |
0 |
1 |
0 |
0 |
0 |
0 |
1 |
0 |
0 |
0 |
|||
Parental relationship |
mother |
15 |
2 |
0 |
0 |
0 |
0,43 |
8 |
7 |
2 |
0 |
0 |
0,72 |
spouse |
3 |
0 |
0 |
0 |
0 |
2 |
1 |
0 |
0 |
0 |
|||
siblings |
2 |
0 |
0 |
0 |
0 |
1 |
1 |
0 |
0 |
0 |
|||
Table 3: Study of the correlation between anxiety scale and the population characteristic’s.
Results and Discussion
Burden measureThe concept of burden refers to “negative effects felt by the person who provide assistance and care”. It concerns what experience the caregiver in relation to his physical, psychological, social and financial condition altering his life at different degrees. The emergence of the term «BURDEN» allows to emphasis the non-professional helpers who support and assist those in need [15]. The median of the measured Burden by Zarit (ZBI) was around 38 with more than half (59%) of cases repots a light to moderate level. These results are comparable to the literature data concerning caregivers of cancer patients, but lower than what have been reported for other diseases; this can be explained by the nature of the studied pathology (Alzheimer, Dementia) and the patient characteristics (elderly, dependent). However, our results are higher than what has been reported in a Turkish series concerning allo-transplanted children where the median ZBI=28, in a comparative English series concerning patients with cancer versus other pathologies, the median ZBI was 23, 3 in the cancer group. Argue that the ignorance of the informal caregiver and the lack of information lead to the expression of greater level of burden. Also, Nazari, et al 2014 prove the place of parental information and its importance in the care process. Since it improves adaptability to the disease and to the decision make, reducing the charge [16, 17].
Population of study and the expressed burdenGender and family relationship: The caregivers were mainly married (86, 4%) and women in about 95%. In 77, 3% it was the mother. Otherwise, it was the wife or the sister in 13, 6% and 4, 5% respectively. Several studies have already described the incredible degree of stigmatization associated with cancer in arab muslim culture. Where cancer has remained a taboo, often nor disclosed to the patient or freely discussed in the family creating a closed circle of care concerning the direct parents (father and mother) and in particular the mother [18]. A Chinese series concerning children with acute lymphoblastic leukemia published in 2017 report 73, 1% of caregivers were mothers, also the Iranian series published in 2019 reported an average of 66%. This may be due to socio economic causes (father at work, housewife), ethical problems (2 women are divorced and keep children) and cultural or ideological factors (the figure of the protective mother) [19].
In our study, gender didn’t modify the ZBI scale due to the disparity in our considered sample=21 women vs. 1 man. Even that, many studies have shown that mothers are the most concerned and are prone to express depression and anxiety; In fact, both parents; the father and the mother experience positive and negative changes in relationships, communication, stress and task distribution [20]. The health care team should avoid excluding any of them, assess the impact of cancer diagnosis and its treatment on parental relationships, offer support and encouragement. Health professional should provide and develop interventions that increase parental potential and enhance their relation during the difficult and long trajectory of cancer and its treatment [21].
Parent’s age: In our study, the median age of parents was 38 years without influence on burden level the same as reported in the Jordanian study published in 2019 with a more large sample(=246 patients). An inverse correlation, has been demonstrated in a recent Iranian study beside another Portugese one where the authors postulate that this opposite relationship is explained by the fact that young parents are new in their parenting experience, are less ready to face this burden and have less possibility of additional resources, especially economic ones [22].
Economic level: Seventy three per cent of cases report subjectively an average level of life without link to Zarit scale (p=0, 66). This may be due in one hand, to the fact that only one items (a single question) is exploring the economic side in this scale and in the other hand, to the presence of an active volunteer association under our department of hematology which covers a large part of the economic needs concerning especially moving between region, treatment and travel cost and accommodation in same case, but for sure biased by the small considered sample [23]. At the opposite to our result, in the literature with large studies, economic factor is considered as a key factor or the main factor that offer a better understanding of the complicated and moving caregiver experience. Financial difficulties are significantly associated with psychological instability and increased burden perception. A low salary is associated with a higher burden which could be explained by the fact that parents of a child with cancer often lose their work. In an Indian study 34% of fathers have lost their job. In our study; 13, 6% of parents lost their job after their children cancer diagnosis. Whereas, it was absent from the beginning in half of cases [24].
The study level: Results concerning this parameter are disparate. While some studies have found a positive correlation between high level of education and low level of burden, others did not report any involvement of education level in parent’s perception of burden. Regarding our population, the study level is superior in 50% of cases without link to the reported burden (p=0,91). But, we considered those results partially biased and other factors are contributing like the length of the interview and the difficulty in collecting information from parents with low study level requiring more time and effort so probable suggestibility bias [25].
Caregiver mental health (study of anxiety) and burden: The caregiver is defined as “any person in the family circle who provides significant support, continuous or occasional, on a non-professional basis, to a person with disability, and in WHO reports as “a family member or friend helping out regularly doing tasks that allow a sick person to maintain as much independence as possible”. The measure of burden as defined by Zarit is interesting because of its link with the mental health of the caregivers. A high burden is generally associated with poor mental and physical health in parents. Which result in higher medication intake such as benzodiazepine abuse, also fatigue, worry and a feeling of helplessness as well as high level of anxiety and depression due to the frequent lack of sleep and exhaustion [26]?
As an example, the degree of depression and anxiety on the Beck and Hamilton scales concerning parents of children with disabilities were respectively 52% and 68% and anxiety were correlated with increased family burden. In a study focused on caregivers of Alzheimer parents Andrieu reported that even a mild to moderate stage of burden causes a particularly harmful character. So, what will be the impact of burden on our studied population? Considering different epidemiological data concerning caregivers (gender, age, family relationship and socioeconomic situation) we notice no relation between mental health and our population characteristics. And only education level seems to act on anxiety state face to such stress (p=0.05). Furthermore, there is no positive relation between reported burden and anxiety (STAI). Parental anxiety level do not exceed an average degree (maximum score=47). Nevertheless, a variation in the level of anxiety was noticed in our study between trait anxiety (AT) and State Anxiety (SA), where AT is in 91% of cases very low to become at 50% low to medium for the AS [27].
These observations could be due to the small sample, and maybe explained in part by the parent passivity and carelessness deduced from this spontaneous expression of burden (moderate to severe in 36% of cases) not aligned with the level of anxiety (very low in more than 50% of cases) and anxiety state modulated only by the level of education. Could there be another aspect linked to depression and social silence? Hence, it is interesting to study other parameters of the mental health in our target population. A study done at the department of radiotherapy Sfax-Tunisia concerning the quality of life of caregiver of cancer patients in 2016 shows; among caregivers: 50.1% had a level of Anxiety State (AS) varying from medium to very high and 76.3% had Anxiety Trait (AT) which ranged from very low to low. The authors deduced that caregiver’s anxiety is not the result of personality trait, but rather is engendered by the situation they were experiencing at the time of study. Looking after a cancer patient presents an anxious condition for the caregiver.
A twelve year Canadian Meta-analysis published in 2013, reported heterogeneous prevalence concerning the mental health of parents of children with cancer. Although it’s higher than what is reported in the general population, the median is about 28% for depression, 26% for post-traumatic stress disorder and 21% for anxiety. Norbey and Bomann in 2007 also reported that the level of anxiety and depression in parents of cancer children exceeds those of parents of healthy ones, especially in the first three months of diagnosis (p<0.001) without gender difference. This may reflect an expected reaction at this stage of disease and treatment. However, about 10% of parents according to the same study express post traumatic disorder even five years after diagnosis. In the latter group, resilience did not occur due to absence of early identification and adequate supports. All these data put emphasize the importance of studies that have involved caregivers as a vulnerable population worthy of screening, monitoring and target interventions.
Impact of the patient and his disease: Parents of children with cancer generally report not only relationship problem but also health problems, leading to more doctors’ consultation. States of distress and post-traumatic stress are often higher in parents than in the patients themselves. They worked on the assumption that no news is good and learned to seek for clues on the non-verbal language of the medical team to guess the severity of the situation. It is now evident that parental stress reduces the chance of resilience in the child/ the patient regarding their adaptability and ability to overcome traumatic events and to hasten their recovery.
So how is the impact of the patient and his disease on the caregiver?
Patient’s gender: Several studies concerning the parent’s burden have studied both genders without showing any significant difference. Parents in our study, mostly mothers, report guilt and anxious concern toward their daughters “Is she going to get married? Will she have children? How are they going to look at her in society? A girl with a cancer!!! You know the girl is not like the boy. She wanted to dress and to do her hair like her friends. She wanted to be spoiled like her sisters”. The distribution in our study was almost balanced 9 girls vs 13 boys but Zarit score was greater (median about 55) among mothers of girls than those of boys (median at 33) with statistically significant difference (p=0.05).
Patient’s age: The median age of patient was 8 year in our study. Often the indication of accompanying hospitalization was indicated by the medical team either with a young child or in an altered health condition. As it has been reported in the literature, the different age groups do not have an impact on the caregiver’s burden level. However, some authors have found that the burden is less when the child is older and they explained this by the fact that the young child requires greater presence of his parents and greater help. In opposite to a mature child who shows a collaborative attitude and dependence (in this study they compared 2 age groups ≤ 13 and >13 years).
Type and status of the disease: Our population is homogenous (it concerns in 95% of cases acute leukemia). Although childhood lymphoblastic leukemia is recognized to have better prognosis compared to myeloblastics, we could not identify any significant difference in the level of expressed burden on our sample related to the type or status of the disease. These results are consistent with what was reported in other studies where even heterogeneous population, the type of the underlying disease does not correlate with burden. The lack of communication and information exchanges between parents and medical team may be in cause. Focusing on symptoms like pain, vomiting. Al Quadire was able to predict the level of parental burden. Could be a lack of communication that had hidden the correlation between the burden and scientific evaluation of the disease? Since several studies have reported that the felt burden is more severe in the advanced stages of the disease.
Hospitalization:The evolution of treatment and especially supportive cares (antibiotics, antifungal, intensive units) mean that doctor’s interest shift from the pure palliative to the hard curative with an extension of hospitalization duration, the frequency of hospitalization and the cost of treatment as a result. Higher levels of burden among the informal caregivers have been reported by H. Kerherve explained by the caregiver-integration-duration, an average 4,4 years for mild to severe stages of Alzheimer’s disease. The same results are found in a longitudinal study conducted by Grunfeld where family caregivers of patients with breast cancer repot a significant level of burden which increases with the progression of the disease.
Our study shows that the disease course is positively correlated with the burden (p=0.004). Obviously, this parent after a long battle alone face to patient needs, finds himself helpless and breathless with an enormous degree of burden. Besides, the number of iterative hospitalizations is correlated to the parental burden (p=0.01) because it reflects not only the evolution of the disease but also the aggressiveness of the pathology (a need for more lines of chemotherapy, presence of more complications). Repetitive hospitalizations disturb intra family relationship with disruption of member’s role and communication within the couple and extra family equilibrium. Frequent hospitalizations exhaust parental resources since they find themselves alone in face of persistent and repeated patient care demands and cause material inventions that the caregiver could not afford (travel, housing, treatment).
Clinical implications and study limitation: This study even was about a small sample with a short period of observation and a need for a tiers person to translate used scales. It still offered a real state and highlight true need for more investigation and exploration of this side (caregiver psychology) of the cancer patients.
Conclusion
Psycho-oncology constitutes a potentially developing field that is interested in the difficulties experienced by the patients and their families. It takes into account in an integrated way the psychological and social impact of the disease and the treatment. Interest in the family dimensions has been developed in psychology, firstly, for the need to implicate relatives in the care after patients in advanced stage, and more recently, for the enormous prevalence of cancer (one in four families has a member with cancer). It seems there is a lot of work to be done and effort to be put into because this subject is not enough treated, although it has a major impact on the outcomes and quality of life for both patients and caregivers. Immediate intervention are compulsory to put in place the necessary measures and solutions, especially when it’s about modifiable factors as the length and the frequency of hospitalization or improvement of study level.
Acknowledgment
- To my dear Professor Raja LABBANE and all her team
- The authors have no conflict of interest to disclosure
References
- Bilani N, Jamali S, Chahine A, Zorkot M, Homsi M, et al. (2019) Illness cognition and health anxiety in parents of children with cancer. J Psychosoc Oncol 37: 713-728.
[Crossref] [Google Scholar] [Pubmed]
- Wang J, Shen N, Zhang X, Shen M, Xie A, et al. (2017) Care burden and its predictive factors in parents of newly diagnosed children with acute lymphoblastic leukemia in academic hospitals in China. Support Care Cancer 25: 3703-3713.
[Crossref] [Google Scholar] [Pubmed]
- Shoghi M, Shahbazi B, Seyedfatemi N. (2019) the effect of the Family-Centered Empowerment Model (FCEM) on the care burden of the parents of children diagnosed with cancer. Asian Pac J Cancer Prev APJCP 20: 1757.
- Motlagh M E, Mirzaei-Alavijeh M, Hosseini S N. (2019) Care burden in parents of children with Leukemia: a cross-sectional study in the west of Iran. Int J Pediatr 7: 9541-9548.
[Crossref] [Google Scholar] [Pubmed]
- Siegel R, L Miller, Kimberly D, Goding Sauer A, Fedewa S A et al. (2020) Colorectal cancer statistics 2020. CA Cancer J Clin 70: 145-164.
[Crossref] [Google Scholar].
- Khazaei S, Khazaei S, Mansori K, Ayubi E. (2017) Childhood cancer patterns in Iran: Challenges and future directions. Iran J Public Health 46: 1145-1146. [Crossref]
- Da Silva FM, Jacob E, Nascimento LC. (2010) Impact of childhood cancer on parents relationships: An integrative review. J Nurs Scholarsh 42: 250-261.
- McGrath P. (2002, July). Beginning treatment for childhood acute lymphoblastic leukemia: Insights from the parents' perspective. Oncol Nurs Forum 29: 988-996.
- Ashok MV, Raman V. (1998). Burden of Care in Parents of Children Suffering from Haematological Malignancies. Indian J Psychiatry, 40: 304-305.
- Nazari S, Moradi N, Koupaei MTS. (2014) Evaluation of the effects of psychotherapy on anxiety among mothers of children with leukemia. Iran J Child Neurol 8: 52-57.
- Spatuzzi R, Giulietti MV, Ricciuti M, Merico F, Fabbietti P, et al. (2019) Exploring the associations between spiritual well-being burden and quality of life in family caregivers of cancer patients. Palliat Support Care PA. 17: 294-299.
[Crossref] [Google Scholar] [Pubmed]
- Jihene BT, Feriel J, Nada C, Lobna Z, Nasreddine Z, et al. (2011) Depression et niveau de fardeau chez les aidants familiaux des sujets dements en Tunisie. Pan Afr med J 10.
- Isokaanta S, Koivula K, Honkalampi K, Kokki H. (2019) Resilience in children and their parents enduring pediatric medical traumatic stress. Pediatric Anesthesia, 29: 218-225.
[Crossref] [Google Scholar] [Pubmed]
- Kerherve H, Gay MC, Vrignaud P. (2008) Sante psychique et fardeau des aidants familiaux de personnes atteintes de la maladie d’Alzheimer ou de troubles apparentes. Ann Med Psychol (Paris) 166: 251-259.
[Crossref] [Google Scholar] [Pubmed]
- Al Qadire M, Aloush S, Alkhalaileh M, Qandeel H, Al-Sabbah A et al. (2020). Burden among parents of children with cancer in Jordan: Cancer Nurs 43: 396-401.
[Crossref] [Google Scholar] [Pubmed]
- Akgul Nur, Leyla Ozdemir. (2014) "Caregiver burden among primary caregivers of patients undergoing peripheral blood stem cell transplantation: a cross sectional study." Eur J Oncol Nurs Eur J 18: 372-377.
[Crossref] [Google Scholar] [Pubmed]
- Hardin R, Gao W, Jackson D, Pearson C, Murray J, et al. (2015). Comparative analysis of informal caregiver burden in advanced cancer dementia and acquired brain injury. J Pain Symptom Manag 50: 445-452.
- Lindahl Norberg A, Boman K K. (2008) Parent distress in childhood cancer: A comparative evaluation of posttraumatic stress symptoms, depression and anxiety. Acta Oncol 47: 267-274.
[Crossref] [Google Scholar] [Pubmed]
- Fekih-Romdhane F, Henchiri H, Ridha R, Labbane R, Cheour M, et al. (2019). Niveau de detresse psychologique et de fardeau perçu chez les conjoints de femmes atteintes d’un cancer du sein. L'Encephale 45: 190-192.
[Crossref] [Google Scholar] [Pubmed]
- Crespo C, Santos S, Tavares A, Salvador A. (2016) “Care that matters”: Family-centered care, caregiving burden, and adaptation in parents of children with cancer. Fam Syst Health FAM 34: 31-40.
[Crossref] [Google Scholar] [Pubmed]
- Wang LJ, Zhong WX, Ji X D, Chen J. (2016). Depression, caregiver burden and social support among caregivers of retinoblastoma patients in China. Int J Nurs Pract 22: 478-485.
[Crossref] [Google Scholar] [Pubmed]
- Ghatak N, Trehan A, Bansal D. (2016) Financial burden of therapy in families with a child with acute lymphoblastic leukemia: Report from north India. Support Care Cancer 24: 103-108.
[Crossref] [Google Scholar] [Pubmed]
- Rha SY, Park Y, Song SK, Lee CE, Lee J, et al. (2015) Caregiving burden and the quality of life of family caregivers of cancer patients: the relationship and correlates. Eur J Oncol Nurs 19: 376-382.
[Crossref] [Google Scholar] [Pubmed]
- Thabet JB, Sallemi R, Hasiri I, Zouari L, Kamoun F, et al. (2013). Repercussions psycho-affectives du handicap de l’enfant sur les parents. Archives de pediatrie 20: 9-16.
- Charfi WM, Jaoua O, Feki I, Masmoudi J, Siala W, et al. (2017) Etude de la qualite de vie de laidant principal des patients en cours de radiothérapie. Cancer Radiother 21: 721-722.
- Van Warmerdam J, Zabih V, Kurdyak P, Sutradhar R, Nathan PC, et al. (2019) Prevalence of anxiety, depression, and posttraumatic stress disorder in parents of children with cancer: A meta‐analy. Ped Blood Can 66: 27677.
[Crossref] [Google Scholar] [Pubmed]
- Grunfeld E, Coyle D, Whelan T, Clinch J, Reyno L, et al. (2004) Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. Cma 170: 1795-1801.
[Crossref] [Google Scholar] [Pubmed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi