Research Article, J Aging Geriatr Med Vol: 5 Issue: 6
Anticholinergic Burden and Hospital Delirium in an Appalachian University Hospital
Shannon Brooke1*, Dhar Romika1 ,Bibb Minta 2, Haghnazar Hameed3,Navia Rosvaldo4 and Thompson James1
1Department of Medicine, West Virginia University, Morgantown, WV, United States.
2Department of Surgery, School of Medicine, West Virginia University, Morgantown, WV, United States.
3Department of Civil Engineering, West Virginia University, United States.
4Department of Medicine, West Virginia University, Morgantown, WV, United States.
*Corresponding Author: Shannon Brooke, Department of Medicine
West Virginia University, Morgantown, WV, United
States.
Tel: +17177985183;
E-mail: brooke.shannon@hsc.wvu.edu
Received: May 06, 2021 Accepted: May 20, 2021 Published:May 27,2021
Citation: Brook e S, Dhar R, Bibb M, Hamed H, Navia RO, et al. (2021) Anticholinergic Burden and Hospital Delirium in an Appalachian University Hospital. J Aging Geriatr Med 5:4.
Abstract
Delirium is a challenging condition in the geriatric inpatient population due to its multifactorial nature. As anticholinergic medications have been observed to be associated with delirium, this association has led to the development of the Anticholinergic Cognitive Burden scale (ACB). Our objective is to determine whether a high ACB score is associated with delirium within an Appalachian population in a West Virginia statewide referral center
Keywords: Anticholinergic Burden, Geriatric Medicine
Abstract
Background: Delirium is a challenging condition in the geriatric inpatient population due to its multifactorial nature. As anticholinergic medications have been observed to be associated with delirium, this association has led to the development of the Anticholinergic Cognitive Burden scale (ACB). Our objective is to determine whether a high ACB score is associated with delirium within an Appalachian population in a West Virginia statewide referral center. Methods: In this retrospective cross-sectional study, 174 patients 65 years or older were assessed with the Confusion Assessment Method (CAM) upon arrival to a general medicine unit at J. W. Ruby Memorial Hospital in Morgantown, West Virginia. The ACB scores were analyzed with reference to presence of delirium per the CAM. Subsequently, ACB scores were compared at two time points— arrival onto the inpatient unit and on the date of discharge. Results: There was no significant association between increased ACB score and presence of delirium. There was no difference in ACB score between patients with and without delirium (p=0.855). When comparing ACB scores on date of CAM versus on date of discharge, there was no significant difference between patients with or without delirium (p=0.467). Conclusion: There was no significant association between a high ACB score and a positive CAM at the time of initial assessment within the limitations of the study. Additionally, there was no change in anticholinergic burden upon patient discharge based on ACB scores.
Keywords
Anticholinergic; Delirium; Anticholinergic Cognitive Burden s cale ( ACB)
Introduction
Delirium is a challenging condition within geriatric inpatient populations and is associated with significant morbidity and mortality. It is a neuropsychiatric syndrome characterized by severe confusion, decline in cognitive ability, inattentiveness, psychomotor disturbances, impaired sleep-wake cycle, and/or emotional and perceptual disturbances [1]. It is estimated that 20% of all hospitalized patients experience delirium at any one time [2]. When delirium occurs among hospitalized elderly patients, it can complicate hospital course and lead to extended stays, worsening cognitive outcomes, inappropriate treatments, distress for the patient and family, and elevated mortality. Additionally, delirium can increase hospital cost by $2500 per patient and $6.9 billion in hospital costs per year [3]. To diagnose delirium, many tools have been developed for quick assessment at the bedside. One such tool is the Confusion Assessment Method (CAM), which is among the most widely used surveys created for non-psychiatrically trained clinicians. It was validated against the Diagnostic and Statistical Manual for Mental Disorders (DSM-V) [4], the CAM has a sensitivity of 94% and specificity of 89% [5]. Risk factors for delirium include: advanced age, prior cognitive impairment, dehydration, fracture, infection, polypharmacy, immobility, restraints, and sensory impairment [6,7]. Prescribed medications have been found to precipitate delirium in between 12%-39% of cases.8 Anticholinergic drugs have detrimental effects on the aged brain because of increased permeability of the blood–brain barrier, slower metabolism and drug elimination, and age-related deficits in central cholinergic transmission [8,9]. Reduced cerebral acetylcholine has been hypothesized to be the common final pathway in the development of delirium in response to inflammation [10]. Hence, in the past few years, research has heavily focused on an association between anticholinergic medications and cognitive impairment in older adults. In a 2008 review of thirteen published longitudinal studies, Boustani et al found that medications with anticholinergic activity were associated with delirium as well as decreased cognitive performance in the acute setting [11]. The results are mixed with regards to relationship between anticholinergic medications and specifically the timing of the onset of delirium. In a recent study of hospitalized adults 65 years and older, the authors found that a higher pre-admission anticholinergic burden was associated with an increased prevalence of delirium [12].However, other studies have observed no association be-tween the administration of anticholinergic medications and the development of delirium in elderly, cancer, or intensive care patients [13-17]. Contrasting results may be explained by limitations to the drug scales themselves as well as population variations. There are multiple scales for assessing anticholinergic burden within the contexts of different populations analyzed. The Anticholinergic Cognitive Burden scale (ACB) was derived in 2008 and validated with other similar scales including those based on physiologic measurement of serum anticholinergic metabolites as well as scales developed by expert opinion and cognitive assessments [18]. The ACB scale uses four qualitative scores from 0 to 3 signifying the effects of anticholinergic use on cognitive impairment. (Tables 1-3) How’s a list of drugs separated into three categories based on cognitive burden. The Anticholinergic Burden scale was chosen for this study as previous studies employing this scale have found an ability to predict cognitive impairment in older adults[18]. Two additional well validated scales that are commonly used include the Anticholinergic Drug Scale as well as the Anticholinergic Risk Scale [18,19]. It is important to note that there is no defined standard scale for assessing anticholinergic burden.
Table 1: Anticholinergic burden scaledrugs with ACB score of 1.
| Generic Name | Brand Name |
|---|---|
| Alimemazine | Theralen ™ |
| Alverine | Spasmonal™ |
| Alprazolam | Xanax™ |
| Aripiprazole | Abilify ™ |
| Asenapine | Saphris™ |
| Atenolol | Tenormin™ |
| Bupropion | Wellbutrin™, Zyban™ |
| Captopril | Capoten™ |
| Cetirizine | Zyrtec ™ |
| Chlorthalidone | Diuril™, Hygroton™ |
| Cimetidine | Tagamet™ |
| Clidinium | Librax™ |
| Clorazepate | Tranxene™ |
| Codeine | Contin™ |
| Colchicine | Colcrys™ |
| Desloratadine | Clarinex™ |
| Diazepam | Valium™ |
| Digoxin | Lanoxin™ |
| Dipyridamole | Persantine™ |
| Disopyramide | Norpace™ |
| Fentanyl | Duragesic™, Actiq™ |
| Furosemide | Lasix ™ |
| Fluvoxamine | Luvox™ |
| Haloperidol | Haldol™ |
| Hydralazine | Apresoline™ |
| Hydrocortisone | Cortef™, Cortaid™ |
| lloperidone | Fanapt ™ |
| Isosorbide | Isordil™, Ismo™ |
| Levocetirizine | Xyzal™ |
| Loperamide | Immodium™, others |
| Loratadine | Claritin™ |
| Metoprolol | Lopressor , Toprol™ |
| Morphine | MS Contin™, Avinza ™ |
| Nifedipine | Procardia™, Adalat™ |
| Paliperidone | Invega™ |
| Prednisone | Deltasone™, Sterapred™ |
| Quinidine | Quinaglute™ |
| Ranitidine | Zantac™ |
| Risperidone | Risperdal ™ |
| Theophylline | Theodur™, Uniphyl™ |
| Trazodone | Desyrel™ |
| Triamterene | Dyrenium™ |
| Venlafaxine | Effexor™ |
| Warfarin | Coumadin™ |
Table 2: Anticholinergic burden scale drugs with ACB score of 2.
| Generic Name | Brand Name |
|---|---|
| Amantadine | Symmetrel™ |
| Belladonna | Multiple |
| Carbamazepine | Tegretol™ |
| Cyclobenzaprine | Flexerilm™ |
| Cyproheptadine | Periactin™ |
| Loxapine | Loxitane™ |
| Meperidine | Demerol™ |
| Methotrimeprazine | Levoprome™ |
| Molindone | Moban™ |
| Nefopam | Nefogesic™ |
| Oxcarbazepine | Trileptal™ |
| Pimozide | Orap™ |
Table 3: Anticholinergic burden scale drugs with ACB score of 3.
| Generic Name | Brand Name |
|---|---|
| Amitriptyline | Elavil™ |
| Amoxapine | Asendin™ |
| Atropine | Sal-Tropine™ |
| Benztropine | Cogentin™ |
| Brompheniramine | Dimetapp™ |
| Carbinoxamine | Histex™, Carbihist™ |
| Chlorpheniramine | Chlor-Trimeton™ |
| Chlorpromazine | Thorazine™ |
| Clemastine | Tavist™ |
| Clomipramine | Anafranil ™ |
| Clozapine | Clozaril™ |
| Darifenacin | Enablex™ |
| Desipramine | Norpramin™ |
| Dicyclomine | Bentyl™ |
| Dimenhydrinate | Dramamine™, others |
| Diphenhydramine | Benadryl™, others |
| Doxepin | Sinequan™ |
| Doxylamine | Unisom™, others |
| Fesoterodine | Toviaz™ |
| Flavoxate | Urispas™ |
| Hydroxyzine | Atarax ™, Vistaril™ |
| Hyoscyamine | Anaspaz™, Levsin ™ |
| Imipramine | Tofranil ™ |
| Meclizine | Antivert™ |
| Methocarbamol | Robaxin™ |
| Nortriptyline | Pamelor™ |
| Olanzapine | Zyprexa™ |
| Orphenadrine | Norflex™ |
| Oxybutynin | Ditropan™ |
| Paroxetine | Paxil™ |
| Perphenazine | Trilafon™ |
| Promethazine | Phenergan™ |
| Propantheline | Pro-Banthine™ |
| Propiverine | Detrunorm™ |
| Quetiapine | Seroquel™ |
| Scopolamine | TransdermScop™ |
| Solifenacin | Vesicare™ |
| Thioridazine | Mellaril™ |
| Tolterodine | Detrol™ |
| Trifluoperazine | Stelazine™ |
| Trihexyphenidyl | Artane™ |
| Trimipramine | Surmontil ™ |
| Trospium | Sanctura™ |
This study was conducted at J. W. Ruby Memorial Hospital which is located in Morgantown, West Virginia. This hospital is a tertiary care academic hospital with 690 beds which serves as a statewide as well as regional referral center for Pennsylvania, Maryland, and Ohio. West Virginia is second in the nation for its aging population with only Florida having a larger population greater than 65 years old. By 2056, the population greater than 65 years old in the US is expected to exceed those less than 17 years old [20]. This change is expected to occur much earlier in West Virginia’s population and is projected to occur by 2029. As of 2013, the Department of Health and Human Resources in WV reported that 1 in 3 households had an adult greater than 65 years old. Concurrently, West Virginia has a higher prevalence of both disability and chronic diseases than the national averages [20]. This population represents an early representation of the aging population within the United States. With this, medical comorbidity and disability rates are high reflecting some of the sickest amongst the aging population in the US.
Methods
This is aretrospective cross-sectional study, which included 174 patients aged 65 years or older who were admitted to J.W. Ruby Memorial Hospital in West Virginia between October 15, 2018 and March 21, 2019. Informed consent was obtained at the time of admission prior to ad-ministration of the CAM. The inclusion criteria for the study were patients over the age of 65 years old admitted to a medicine floor. The exclusion criteria included those patients undergoing detoxification for substance abuse, prisoners, comatose, actively dying, and lack of CAM documentation by the bedside nurse. Patients were chosen as part of a previous study conducted at this hospital assessing inpatient delirium and CAM scores. The patients were assessed for delirium with the CAM upon arriving to a regular medicine floor regardless of whether they showed delirium symptoms. Patient electronic medical records were reviewed for age, principal diagnoses, inpatient medications on date of CAM, chronic diseases, kidney and liver function tests, and additional contributing factors for delirium. Subjects were divided into delirium-positive and delirium- negative groups based on the results of the CAM. Using the most current medication list from the date of the CAM, a cumulative ACB score was derived. The primary endpoint was to determine the ACB score amongst both delirium positive and delirium negative patients. A clinically significant ACB score was defined as greater than three. The percentage of delirium positive patients with a clinically significant ACB score was compared to delirium negative patients with a clinically significant ACB score. Numerical data was used for ACB score means rather than positive or negative ACB score because many patients were noted to have ACB scores ranging between 2-4 and the difference was better reflected by numerical averages rather than categorical assessment. A subsequent analysis compared ACB score on the date of the CAM administration versus ACB score on the date of discharge. In this dataset, five patients died before discharge and were thus excluded. Differences in ACB scores were compared with the Mann- Whitney U test. Reported medians and non-parametric confidence intervals were generated in R Hodges-Lehmann estimator. We hypothesized that if a patient was positive for delirium by CAM, then they would have a significant anticholinergic burden (ACB>3). Additionally, we hypothesized that the anticholinergic burden would have been reduced at the time of discharge.
Results
The data suggested no difference in ACB score between patients with and without delirium (p=0.855) at the time of CAM administration. ACB scores ranged from 0-11, with roughly 75.3% of patients on at least one anticholinergic medication. (Table 4) illustrates this comparison. The mean ACB score among delirium negative patients was 2.08 while the mean ACB score for delirium positive patients was 2.23.
Table 4: Anticholinergic burden score (ACB) scores on date of the confusion assessment method (CAM).
| Presence of Delirium per CAM | Number of patients (n) | Median | 95% CI | p-value |
|---|---|---|---|---|
| No | 134 | 2.5 | 2, 3 | |
| Yes | 40 | 2.5 | 2, 3.5 | 0.855 |
Demographic data was collected and included: mean age, gender, number of days hospitalized before CAM test was performed, total length of stay, and patient origin (Table 5). To determine the impact of possible confounding variables, several potential risk factors were compared between groups. Those variables included possible precipitating factors for serum anticholinergic activity such as renal function as well as other known causes of delirium such as infection, stroke/TIA, myocardial infarction, and illicit drug/alcohol intoxication. Neither was overrepresented with any one potential precipitating variable (Table 6).
Table 5: Sociodemographic characteristics of patients stratified based on presence of delirium per Confusion Assessment Method (CAM).
| Characteristic | (-) Delirium | (+) Delirium | p-value |
|---|---|---|---|
| Number of patients | 134 | 40 | 1 |
| Age (years; mean ± SD) | 75.77 ± 7.625 | 73 ± 7.31 | 0.574 |
| Female (%) | 55% | 46% | 0.469 |
| Number of dayshospitalizedbefore date of CAM (mean) | 2.4 | 2.8 | 0.731 |
| Total length of stay | 5.62 | 6.81 | 0.773 |
| Patient originprior to CAM | 0.362 | ||
| Anotherinpatientward | 34.30% | 41.50% | |
| Home | 43.30% | 36.60% | |
| Skilled nursing facility | 3.00% | 7.30% | |
| Outsidehospital | 19.40% | 12.20% |
Table 6: Potential confounding variables.
| Variables | (-) Delirium | (+) Delirium | p-value |
|---|---|---|---|
| BUN (mean ± stddev) | 23.91 ± 16.07 | 23.90 ± 14.65 | 0.997 |
| Creatinine | 1.48 ± 1.23 | 1.45 ± 1.05 | 0.905 |
| Total Bilirubin | 182% | 165% | 0.871 |
| Conjugated Bilirubin | 1.028 | 0.873 | 0.774 |
| Albumin | 2.77 ± 0.83 | 3.00 ± 0.83 | 0.213 |
| AST | 58.56 | 42.15 | 0.271 |
| ALT | 5189.00% | 6785.00% | 0.551 |
| Alkaline Phosphatase | 14939.00% | 11254.00% | 0.106 |
| Urine Drug Screen | 2.24% | 2.50% | 0.923 |
| Benzodiazepine within 48 hours of CAM | 8.96% | 12.50% | 0.508 |
| Opioids within 48 hours of CAM | 0.2761 | 0.325 | 0.549 |
| Recent Stroke/TIA | 0.0373 | 0.1 | 0.116 |
| Recent Surgery | 0.1716 | 0.175 | 0.961 |
| Recent Heart Attack | 0.0522 | 0.075 | 0.587 |
| Active Infection | 0.4701 | 0.45 | 0.823 |
| Underlying Dementia | 0.1716 | 0.075 | 0.132 |
Additionally, an ACB score was calculated at the time of discharge for comparison to the day of CAM administration. This was completed to assess if the anticholinergic burden had been reduced at the time of discharge. Tables 5 and illustrate these results. Patients who were delirium-positive and had not died before discharge totaled 36. In this group, the mean ACB on the date the CAM was 2.23, while the mean ACB score on the date of discharge was 2.50. There was no statistically significant change in ACB score by the date of discharge (p=0.738).
Discussion
Results from our study did not show an association between anticholinergic cognitive burden and the diagnosis of delirium. Delirium often has multiple precipitating factors and rendering an obvious solitary association is difficult to ascertain. The ACB scoring system was devised as a tool to help with accounting for anticholinergic effects of certain commonly used pharmaceutical agents. However, our study suggests that application of the tool would not benefit in guiding identification of the cause of delirium nor justify the reduction of a patient’s anticholinergic medications to treat their delirium. Critiques of using drug scales are that the cumulative exposure to anticholinergic medications are oversimplified into linear additive models and these scales do not necessarily consider the underlying patient characteristics including differences in pharmacodynamics, cholinergic reserve, and endogenous anticholinergic activity [21]. Within this population, comorbidity alone may present a unique challenge to identifying anticholinergic burden as a factor contributing to the presence of delirium. In reviewing the data, it was noted that many patients automatically scored higher on their ACB score based on their comorbidities. For example, many patients with diagnosed heart failure automatically had a score of two due to use of both metoprolol as well as furosemide. Additionally, digoxin and hydralazine were commonly present on their medication lists and will also raise the score. The degree of multimorbidity in this population may make it difficult to analyze a solitary contributing factor to the presence of delirium. West Virginia ranks third in the nation by definition for multiple chronic medical conditions. Multiple chronic conditions are defined as two or more of the following group (arthritis, asthma, cancer, COPD, coronary heart disease, diabetes, hepatitis, hypertension, stroke or weak or failing kidneys). This population notably does not reflect significant ethnic diversity as the 2013 WV DHHR data indicates the state is 96.7% Caucasian [20]. Additional limitations of this study include the small sample size of patients that were diagnosed with delirium. Forty patients who were diagnosed with delirium out of 174 total patient electronic medical records analyzed composes roughly 23% of the entire sample. The small sample size lead to a lower powered study and it is possible that a larger sample size would yield different results. Additionally, the small sample size made stratification for analyzing confounding variables challenging as there were not a sufficient number of patients with delirium to investigate other effects. Also, the anticholinergic usage was detected using medication orders rather than actual dispensing data, which could inform about whether the exposure was relatively new or cumulative over a prolonged period of time. One more complexity of this study that differs from other studies is that no cutoff for anticholinergic burden was selected, but rather the ACB scores were treated as a continuous numerical variable. Research groups that put an absolute cutoff for maximum anticholinergic value showed significant associations between anticholinergic burden and delirium. For example, Pascina and colleagues showed in 2012 a relationship between ACB scores and Short Blessed Test (SBT), which had previously been validated against the Mini-Mental State Exam (MMSE) by Carpenter et al in 2011 [22,23]. Future directions for similar studies ought to significantly increase sample size to better represent the population. Analysis of the ADS and ARS may prove to have different outcomes for example.
Conclusion
The growing population of elderly patients may necessitate refined tools for quick and early diagnosis of acute mental changes including those potentially caused by the anticholinergic effects of common medications. It is important to identify the acute negative impact that polypharmacy has on the aging brain especially amongst an aging and medically complex population. Therefore, there is value in identifying tools that allow clinicians to quickly determine whether an acutely delirious patient may benefit from reducing anticholinergic burden. The relationship between delirium, anticholinergic burden scores, and acetylcholine levels or serum anti-cholinergic levels should be investigated further. More studies are thus needed to identify such tools as well as establish therapeutic guidelines in dealing with delirium. Therefore, evidence-based tools such as the ACB need continued validation in order to reliably change practice.
References
- Vihang NV (2013) Diagnostic and statistical manual of mental disorders. Am J Psychiatry 55: 220-223.
- Ryan DJ, Regan ONA, Caoimh RÓ, Claire J, Conner OM, et al. (2013) Delirium in an adult acute hospital population predictors prevalence and detection. BMJ Open 3: 1-9.
- Leslie DL, Zhang Y, Edward RM (2008) One-year health care costs associated with delirium. Arch Intern Med 8: 27-32.
- Chanques G, Ely EW, Garnier O, Fanny P, Anaïs E, et al. (2018) The 2014 updated version of the confusion assessment method for the intensive care unit compared to the 5th version of the diagnostic and statistical manual of mental disorders and other current methods used by intensivists. Ann Intensive Care 8: 1-10.
- Wei LA, Fearing MA, Sternberg EJ, Inouye SK (2008) The confusion assessment method (CAM): a systematic review of current usage. J Am Geriatr Soc 56: 823-830.
- Lau T, Kozyra E, Cheng C (2019) Delirium risk factors, contributors, identification, work-up, and treatment. Am J Geriatr Psychiatry pp: 219-235.
- Schor JD, Levkoff SE, Lipsitz LA, Reilly CH, Cleary PD, et al. (1992) Risk factors for delirium in hospitalized elderly. JAMA 267: 827-831.
- Alagiakrishnan K, Wiens CA (2004) An approach to drug induced delirium in the elderly. Postgrad Med J 80: 388-393.
- MintzerJ, Burns A (2000) Anticholinergic side-effects of drugs in elderly people. J R Soc Med 93:457-462.
- VanGool W, Van de Beek D, Eikelenboom P (2010) Systemic infection and delirium: when cytokines and acetylcholine collide. Lancet 375: 773-775.
- Boustani, M, Campbell N, Munger S, Maidment I, Fox F, et al. (2008) Impact of anticholinergics on the aging brain: a review and practical application. Aging Health 4: 311-320.
- Rigor J, RueffRato I, Ferreira P, Pereira R, Ribeiro C, et al. (2020) Pre hospital anti cholinergic burden is associated with delirium but not with mortality in a population of acutely Ill medical Patients. J Am Med DirAssoc 21: 481-485.
- Luukkanen MJ, Uusvaara J, Laurila JV, Strandberg TE, Raivio MM, et al. (2011) Anticholinergic drugs and their effects on delirium and mortality in the elderly. Dement GeriatrCogn Dis Extra 1: 43–50.
- Campbell N, Perkins A, Hui S, Khan B, Boustani M (2011) Association between prescribing of anticholinergic medications and incident delirium: acohort study. J Am Geriatr Soc. 59: S277–S281.
- Pasina L, Colzani L, Cortesi L, Tettamanti M, Zambon A, et al. (2019) Relation between delirium and anticholinergic drug burden in a cohort of hospitalized older patients: an observational study. Drugs Aging 36: 85-91.
- Moorey HC, Zaidman S, Jackson TA (2016) Delirium is not associated with anticholinergic burden or polypharmacy in older patients on admission to an acute hospital: an observational case delirium-negative study. BMC Geriatr 16: 162.
- Gaudreau JD, Gagnon P, Harel F, Roy MA, Tremblay A, et al. (2005) Psychoactive medications and risk of delirium in hospitalized cancer patients. J Clin Oncol 23: 6712–6718.
- SalahudeenMS, Duffull SB, Nishtala PS (2015) Anticholinergic burden quantified by anticholinergic risk scales and adverse outcomes in older people: a systematic review. BMC Geriatr 15: 31.
- Carnahan RM, Lund BC, Perry PJ, Pollock BG, Culp KR (2006) The anticholinergic drug scale as a measure of drug-related anticholinergic burden associations with serum anticholinergic activity. J Clin Pharmocal 46: 1481-1486.
- West Virginia Department of Health and Human Resources, Bureau for Public Health, Health Statistics Center (2016). West Virginia’s Aging Population, 1950 to 2013.
- Kersten H, Wyller TB (2014) Anticholinergic drug burden in older people’s brain how well is it measured. Basic Clin Pharmacol Toxicol 114: 151–159.
- Pasina L, Djade C, Lucca U, Nobili A, Tettamanti M, et al. (2012) Association of anticholinergic burden with cognitive and functional status in a cohort of hospitalized elderly: comparison of the anticholinergic cognitive burden scale and anticholinergic risk scale. Drugs Aging 30: 103-112.
- Carpenter CR, Bassett ER, Fischer GM, Shirshekan J, Galvin JE, et al. (2011) Four sensitive screening tools to detect cognitive dysfunction in geriatric emergency department patients: brief alzheimer’s screen, short blessed test, Ottawa 3dy, and the caregiver-completed ad 8. J Acad Emerg Med 18: 374–384.
Track Your Manuscript
Explore SciTechnol
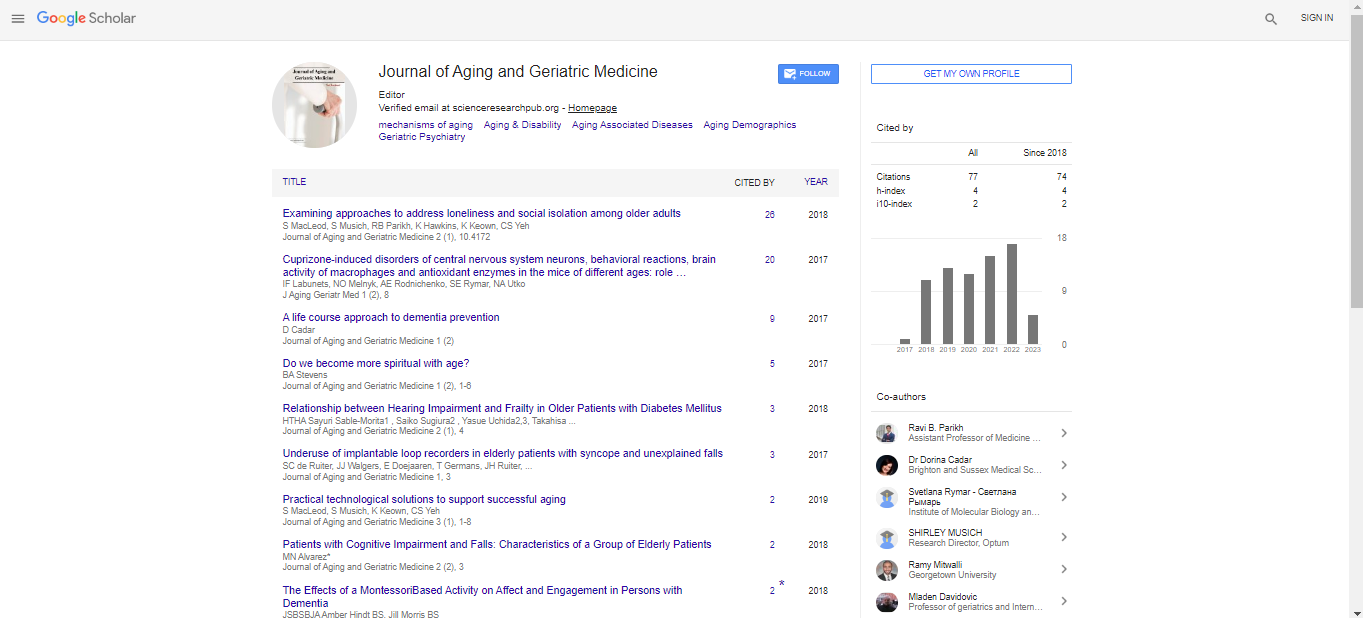
Google Scholar citation report
Citations : 77
Journal of Aging and Geriatric Medicine received 77 citations as per Google Scholar report
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi