Research Article, Clin Res Orthop Vol: 3 Issue: 1
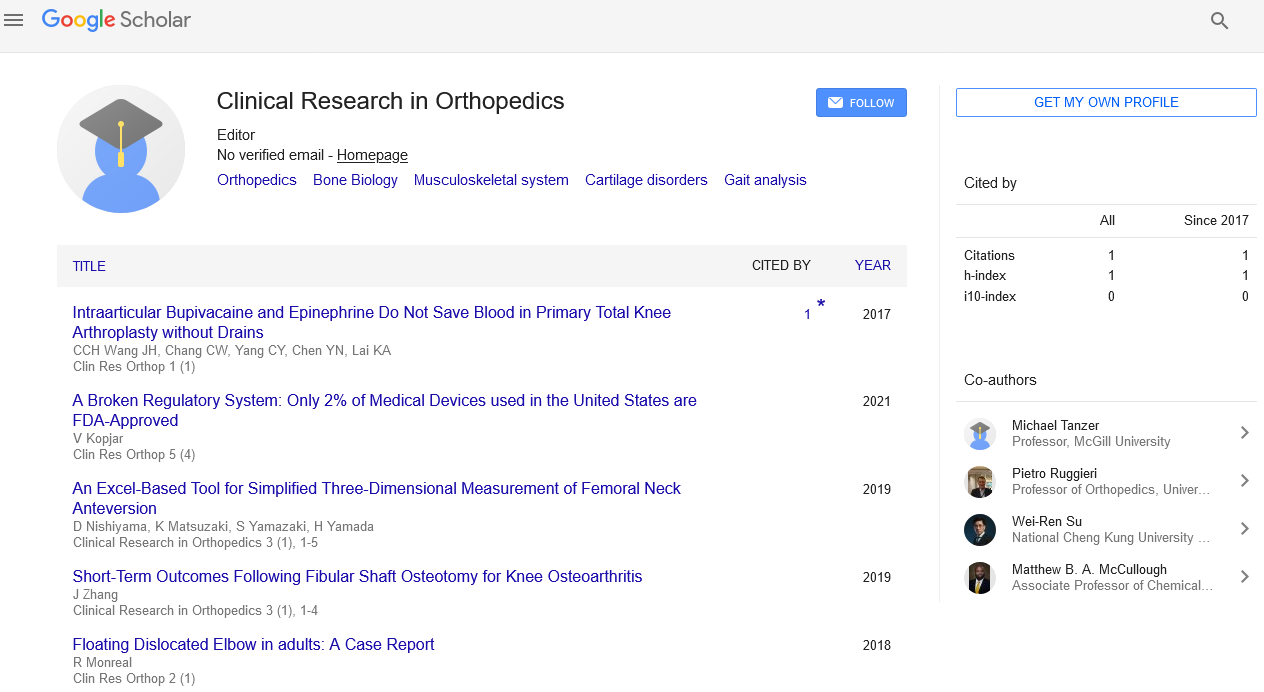
An Excel-Based Tool for Simplified Three-Dimensional Measurement of Femoral Neck Anteversion
Daisuke Nishiyama*, Kosaku Matsuzaki, Satoru Yamazaki and Hiroshi Yamada
Department of Orthopaedic Surgery, Wakayama Medical University, Wakayama, Japan
*Corresponding Author : Daisuke Nishiyama
Department of Orthopaedic Surgery, Wakayama Medical University 811-1 Kimiidera, Wakayama, 641-0012, Japan
Tel: +81-73-441-0645
E-mail: nishinishiminami2000@yahoo.co.jp
Received: August 14, 2019 Accepted: September 11, 2019 Published: September 16, 2019
Citation: Nishiyama D, Matsuzaki K, Yamazaki S, Yamada H (2019) An Excel-Based Tool for Simplified Three-Dimensional Measurement of Femoral Neck Anteversion. Clin Res Orthop 2:2.
Abstract
Objective: We devised a simple three-dimensional (3D) application for femoral neck anteversion (AV) measurement using cross-sectional computed tomography (CT). To assess the accuracy and reproducibility of this method, we compared it with two previously established cross-sectional CT methods.
Materials and methods: AV measurements using CT were performed on 11 consecutive patients before primary total hip replacement for osteoarthritis. The mean age was 72 years (range, 53-81 years); all patients were females. Inter- and intraobserver variabilities were assessed. The measurement times of each method were compared. The correlations with the results obtained using 3D modeling software were also assessed.
Results: Interobserver reliability measured as the intraclass correlation coefficient (ICC) was 0.89, 0.84, and 0.76 for the method of Reikeras et al., the single-slice method, and our method, respectively. The intraobserver reproducibility of all the methods was excellent (range, 0.86-0.97). AV measurements using the 3D modeling software positively correlated with the single slice method (r=0.70) and the method of Reikeras et al. (r=0.60). Notably, the positive correlations with our method were excellent (r=0.93). Measurement time of this method was significantly longer than the other methods.
Conclusion: This simplified method achieves a good level of accuracy and reproducibility. This method can be used in clinics with no access to 3D measurements.
Keywords: Cubosome; Cubosomal gel; Ketoprofen; Top- down technique
Introduction
In the management of osteoarthritis of the hip, developmental dysplasia of the hip, and femoral neck fractures, accurate measurement of femoral neck anteversion (AV) is critical. Femoral neck AV measurement is also essential for total hip replacement (THR) planning. Numerous methods for measuring AV have been developed. Murphy et al. [1] described an accurate computed tomography (CT) method for measuring AV in the femoral neck. Currently, the CT method is the method of choice [2,3].
Application of the CT method requires the long axis of the femoral diaphysis to be positioned perpendicular to the direction of sectioning [1]. However, many patients suffering from hip disorders have difficulty in positioning because of pain or joint contracture. Incorrect position of the patient, with inexact abduction, lexion, and rotation of the hip, in luences femoral neck AV calculations [4,5].
The three-dimensional (3D) CT method does not depend on the actual femoral position and achieves an accuracy of 1° [6]. Comparison of AV measurements using 3D hip reconstruction with the femoral neck AV measurement from the CT section shows that the 3D measurements are more accurate [7]. Recently, clinical environments where 3D modeling is unavailable are becoming increasingly rare, but there are quite a few clinics that lack special software for accurate 3D measurements. Although 3D reconstruction provides the most accurate measurement of femoral neck AV without the influence of position, its complexity and/or expense make it inaccessible to the majority of surgeons [6]. Furthermore, 3D imaging requires more CT sections, subjecting the patient to higher radiation dosages [5].
We devised a simple computer application for the 3D measurement of femoral neck AV using cross-sectional CT images focusing on the differences between the direction of the proximal femoral shaft axis and the longitudinal axis in CT (Z-axis, slice thickness direction). The application was designed using Microsoft Excel.
The purpose of this study was to assess the accuracy and reproducibility of this method by comparing it with two previously established cross-sectional CT methods. Furthermore, we compared the measurement times and investigated the correlation coefficients with the results obtained from 3D modeling software.
The two previous established methods are as follows: (a) the classic single-slice CT method, in which the neck axis is determined from single cross-sectional CT image [8] and (b) the method designed by Reikerås et al., [4] in which the neck axis is determined from the superimposed image of the femoral head and neck.
Materials and Methods
This was an institutional review board-approved prospective study of patients undergoing an elective primary THR from October to December 2013. Preoperative bilateral 2D and 3D CT AV measurements were performed on 11 consecutive patients before THR for nontraumatic osteoarthritis. Exclusion criteria included previous THR or osteotomy and ipsilateral above-knee amputation. Consequently, three hips were excluded because of previous THR. The remaining 19 hips were investigated in this study. The mean age was 72 years (range, 53-81 years); all patients were females. The primary diagnosis was osteoarthritis in 13 hips, and 6 hips were radiographically normal. All subjects were examined in the supine position with the hips and knees extended, and lower limps horizontally parallel as much as possible.
In the abovementioned cross-sectional CT methods (a, b), the femoral neck AV was defined as the angle between the neck axis and the tangential line joining the most posterior aspect of the lateral and medial condyles.
For the single-slice method, the neck axis was defined as the line passing through the midpoints of the neck at both the medial and lateral edges of the central portion of the neck at the slice just below the inferior edge of the head [8] (Figure 1).
For the head-neck superimposition method of Reikerås et al., [4] the neck axis was defined as the line passing through the center of the femoral head and midpoint of the narrowest diameter of the neck at the slice through the middle of the femoral neck (Figure 2).
In the 3D modeling software, femoral neck AV was defined as the angle between the neck axis and the condylar line projected onto a plane perpendicular to the proximal femoral shaft axis. The neck axis was defined as the perpendicular line from the center of the femoral head to the proximal femoral shaft axis. The axis of the proximal femoral shaft was obtained as the line of best fit through centroids of transverse slices taken just below the lesser trochanter to the femoral canal isthmus. The condylar line was determined as the tangential line joining the dorsal aspects of the femoral condyles.
In this simplified 3D method, the femoral neck AV comprised the upper and lower part of AV. The upper part of AV was defined as the angle between the neck axis and the horizontal line projected onto a plane perpendicular to the proximal femoral shaft axis (Figure 3). The neck axis was defined as the perpendicular line from the center of the femoral head to the proximal femoral shaft axis. The proximal femoral shaft axis was obtained as the line passing through the centroid of the cross-section taken just below the lesser trochanter and the centroid of the femoral canal isthmus. The lower part of AV was defined as the angle between the horizontal line and tangential line joining the most posterior aspect of the lateral and medial condyles in the crosssectional CT image of condyles. The lower part of AV was positive when the knee was rotated inwards and negative when the knee was rotated outwards. The horizontal line was obtained as the line parallel to the table of the scanner in the cross-sectional CT image.
Figure 3: Definition of the upper part of the AV (θu) in this method. The proximal femoral shaft axis (O-I) defines plane α; a plane perpendicular to O-I. θu was defined as the angle between the neck axis and the horizontal line projected onto the plane α. The neck axis was defined as the perpendicular line from H to O-I. AV, anteversion; H=the center of the femoral head. O=center of the proximal femoral shaft at the level just below the lesser trochanter. I=center of the femoral canal isthmus.
CT scans of 19 femurs were obtained using a helical CT scanner (LightSpeed VCT 64 detector; GE, Milwaukee, WI, USA), in helical mode with slice thickness set at 2.5 mm, and reconstructed using software. Images were reviewed using Synapse software (FUJIFILM Medical Co. Ltd., Tokyo, Japan). CT-based reconstruction software was used to create virtual three-dimensional (3D) bone models and define the axis of the femoral neck, using a pre-operative THR planning mode (ZedHip; LEXI Co. Ltd., Tokyo, Japan).
To evaluate interobserver variation, all AV measurements were independently performed by three orthopedic surgeons. To determine intraobserver variation, the measurement was repeated after four weeks by one orthopedic surgeon. Measurement times were recorded by a blinded examiner who was not involved in the AV measurement. The measurement times of each method were compared. The correlations with the results obtained using the 3D modeling software were assessed.
Imaging method
Measurements for this method were performed referring to the CT coordinates used in the method proposed by Hermann and Egund [5]. For the measurement of the upper part of the AV, the proximal femoral shaft axis O-I was constructed (Figure 3). The proximal femoral shaft axis was defined from the center of the proximal femoral shaft at the level just below the lesser trochanter (O) and the center of the femoral canal isthmus (I). His the distance from the center of the femoral head(H) to the lateral edge of the CT image. H is the distance from H to the lower edge of the CT image (Figure 4). Similarly, the , coordinates of the reference points (O, I) were measured. Slice numbers of the CT image taken through each reference points (H, O, and I) were recorded. The distance of the z-axis between each reference points was obtained from the product of the slice thickness and the difference of slice numbers.
Figure 4: Definition of the x,y coordinates of the reference points. Hx is the distance from H to the lateral edge of the CT image. Hy is the distance from H to the lower edge of the CT image. Similarly, the x,y coordinates of the reference points (O,I) were measured. H=the center of the femoral head. O=the center of the proximal femoral shaft at the level just below the lesser trochanter. I=the center of the femoral canal isthmus.
The lower part of AV defined as the angle between the horizontal line and the tangential line joining the most posterior aspect of the lateral and medial condyles was directly measured in the crosssectional CT image of condyles.
Calculations
The upper part of the AV was calculated by applying the inner product of orthogonal projection vectors, which are the neck axis and the horizontal line projected onto a plane perpendicular to the proximal femoral shaft axis.
All calculations were obtained using a Microsoft Excel worksheet that we programmed. The acquired values were completed for cells B2:E4, respectively. The Excel program used is in Table 1. Thereafter, the upper and lower parts of the AV are summated.
Statistical analysis
The Shapiro-Wilk normality test was used in advance to confirm the normal distribution of variables. For multiple comparisons among the measurement times of each method, the Steel-Dwass test was used.
The interobserver and intraobserver repeatability analysis was performed by calculating the intraclass correlation coefficients (ICCs). The ICC values were categorized as follows: <0.40, poor to fair agreement; 0.41–0.60, moderate agreement; 0.61–0.80, good agreement; and 0.81–1.00, excellent agreement [9].
Pearson’s correlation coefficient was used to investigate any correlations between AV measurements using cross-sectional CT methods and AV measurements using the 3D modeling software. The magnitude of correlation was based on Cohen’s criteria: 0 to 0.1, trivial correlation; 0.1 to 0.30, small correlation; 0.30 to 0.50, moderate correlation; 0.50 to 0.70, indicated large correlation; 0.70 to 0.90, very large correlation; and >0.90, close to perfect [10].
All statistical analyses were performed using JMP 8.0.2 statistical software (SAS Institute Inc., North Carolina, USA) and Excel Microsoft Office 2007. Statistical significance was defined as p<0.05.
Results
As shown in Table 2, the measurement time of our method was significantly longer than the other two methods (p<0.05).
| Method of calculation | This method (simplified 3D reconstruction) | Single slice | Head-neck superimposition (Reikerås) |
|---|---|---|---|
| Anteversion (mean ± SD, deg | 39.2 ± 7.2 | 17.1 ± 10.4 | 14.5 ± 8.2 |
| measurement time (med ± QD, sec | 258 ± 20.1* | 85.5 ± 14.4 | 91 ± 8 |
| ICC 1,2 (intra-observer) | 0.91 | 0.97 | 0.86 |
| ICC 2,1 (inter-observer) | 0.76 | 0.84 | 0.89 |
| correlation with results of the 3D modeling software | 0.93 | 0.7 | 0.6 |
Table 2: Summary of comparison among three cross-sectional CT methods for anteversion measurement
The interobserver reliability measured as the ICC was 0.89 for the method of Reikerås et al. and 0.84 for the single-slice method, indicating excellent reproducibility, whereas ICC for our method was 0.76, indicating good reproducibility. The results of the analysis of intraobserver reliability are summarized in Table 2. The intraobserver reproducibility of all measurement methods was excellent, with ICC ranging from 0.86 to 0.97.
SD=standard deviation; deg=degree; Med=Median; QD=quartile deviation; sec=second; ICC=intraclass correlation coefficient (*: p<0.05).
Table 2 shows the correlation coefficients between AV measurements using the 3D modeling software and AV measurements using the three different types of cross-sectional CT methods. AV measurements using the 3D modeling software positively correlated with the single slice method (r=0.70, p<0.01) and the method of Reikerås et al. (r=0.60, p<0.01). “Nearly perfect” positive correlations were obtained with our method (r=0.93, p<0.01).
Discussion
Murphy’s CT method requires the long axis of the femoral diaphysis to be positioned perpendicular to the direction of sectioning [1]. Many other CT methods have proven to be reliable only in the examination of femoral specimens positioned similarly. Incorrect hip position influenced the calculations of femoral neck AV. Hermann et al. [5] reported the influence exerted by different femoral shaft positions. The results of this simplified 3D measurement strongly correlate with the results obtained by the 3D modeling software, which did not depend on the actual femoral position. Thus, suggesting this method to be appropriate.
Concerning CT coordinates; reference point O was defined as the center of the base of the femoral neck at the level of the lesser trochanter according to the study by Murphy et al. However, we modified the definition of reference point O to the center of the proximal femoral shaft at the level just below the lesser trochanter, so that the reproducibility is improved in the unreconstructed scan data. The results of this study suggest that our attempt was successful.
Because the main purpose of this study was to assess the reproducibility of various methods, we did not compare the value of AV. Comparison of the results of the different definitions has little meaning. However, a mean value of 39° of this method, which is very different from those of other two previous methods, may attract the reader’s attention.
The reason for this is as follows:
Bonneau et al. showed that the femoral neck axis and the femoral shaft axis do not intersect [11]. The femoral neck axis crosses above the femoral shaft axis, and the minimal distance between these two axes is 4.9 mm on average. Furthermore, the minimal distance will be extended by the influence of the antecurvature of the femur when the femoral shaft axis replaces the proximal femoral shaft axis. Although the distance does not influence the results of AV in the methods that measure an angle between the femoral neck axis and the condylar line, an angle equal to the distance is added in this method, which calculates the positional relation of the (proximal) femoral shaft axis and the center of the femoral head.
The mean AV obtained by the 3D modeling software was 37.6 ± 6.9°, which is similarly calculated from the positional relation of the proximal femoral shaft axis and the center of the femoral head. The proximal femoral shaft axis is not a weight-bearing axis but is an invaluable reference axis, which can be directly confirmed in an operative field.
This simplified 3D method involved the consideration of several issues. First, this method is not 3D measurement in the true sense of the term. The lower part of AV was directly obtained in the crosssectional CT image of condyles. If the lower part of AV was additionally calculated from coordinates of most posterior aspects of the lateral and medial condyles, it can be said that this method is an authentic 3D measurement method. However, it sacrifices the practicality of this method. Although the lower part of AV obtained in the cross-sectional CT image had been used as a substitute for 3D measurement in this method, the results of this method strongly correlate with the results obtained by the 3D modeling software.
Secondly, the interobserver reliability of this method was slightly lower than the other methods. In cases that present with a severe degree of collapse and deformity of the femoral head, it is even more difficult to specify a center point of the femoral head. However, the difference from the method of Reikerås et al., which also used the center of the femoral head as a reference point, suggests involvement of other factors.
Thirdly, we adopted a certain definition for 3D AV in the 3D modeling software as the object of comparison in the present study. In the absence of a gold standard for the definition of 3D AV, various definitions have been used. Provided that the other proposed definitions of the neck axis were adopted, e.g., the line of best fit through the centroids of femoral neck slices, different results were expected.
Finally, this study excluded patients with severe contracture of the hip joint. Concerning the severity of hip subluxation, all investigated hips were classified as either normal or Crowe type I. An additional investigation targeting patients with severe hip contracture is necessary.
For a slightly complicated procedure, the measurement time of our method was significantly longer than the other two methods. But a measurement time of 258 seconds (on average) in exchange for high accuracy and reproducibility is acceptable in practicality.
Conclusion
This simplified 3D method for AV measurement achieves a high accuracy and reproducibility. The results of this simplified method more strongly correlate with the highly reliable results obtained by the 3D modeling software than two previously established cross-sectional CT methods. Utilizing this simplified method may also be cost effective compared with 3D modeling software, which requires advanced computer console devices. Where there is no access to measurements of 3D reconstruction models in the clinical environment, this simplified method is appropriate and practical.
References
- Murphy SB, Simon SR, Kijiewski PK, Wilkinson RH, Griscom NT (1987) Femoral anteversion. J Bone Joint Surg Am 69: 1169-1176.
- Tayton E (2007) Femoral anteversion: A necessary angle or an evolutionary vestige? J Bone Joint Surg Br 89: 1283-1288.
- Delialioglu MO, Tasbas BA, Bayrakci K, Daglar B, Kurt M, et al. (2006) Alternative reliable techniques in femoral torsion measurement. J Pediatr Orthop 15: 28-33.
- Reikeras O, Bjerkreim I, Kolbenstvedt A (1982) Anteversion of the acetabulum in patients with idiopathic increased anteversion of the femoral neck. Acta Orthop Scand 53: 847-852.
- Hermann KL, Egund N (1997) CT measurement of anteversion in the femoral neck. The influence of femur positioning. Acta Radiol 38: 527-532.
- Egund N, Palmer J (1984) Femoral anatomy described in cylindrical coordinates using computed tomography. Acta Radiol Diagn (Stockh) 25: 209-215.
- Abel MF, Sutherland DH, Wenger DR, Mubarak SJ (1994) Evaluation of CT scans and 3-D reformatted images for quantitative assessment of the hip. J Pediatr Orthop 14: 48-53.
- Sugano N, Noble PC, Kamaric E (1998) A comparison of alternative methods of measuring femoral anteversion. J Comput Assist Tomogr 22: 610-614.
- McGraw KO, Wong SP (1996) Forming inferences about some Intraclass Correlation Coefficients. Psychol Methods 1: 30-46.
- Cohen J (1988) Statistical Power Analysis for the Behavioral Sciences (2nd edn) Lawrence Erlbaum Associates, New Jersey, USA.
- Bonneau N, Libourel PA, Simonis C, Puymerail L, Baylac M, et al. (2012) A three-dimensional axis for the study of femoral neck orientation. J Anat 221: 465-476.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi