Research Article, J Plast Surg Cosmetol Vol: 1 Issue: 1
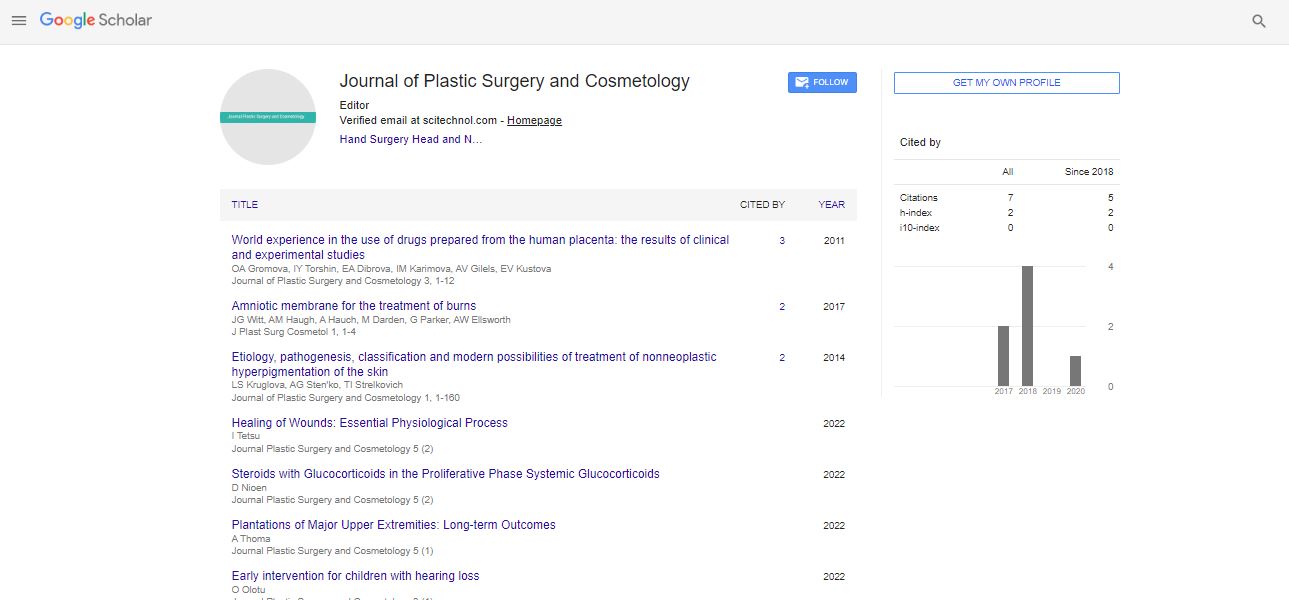
Amniotic Membrane for the Treatment of Burns
Jacqueline G Witt1, Alexandra M Haugh1, Adam Hauch MD1, Michael Darden2, Geoffrey Parker3, Warren A Ellsworth3 and Joseph F Buell1*
1Tulane University, New Orleans, Louisiana
2Milken Institute of Health Care Policy, George Washington University, Washington DC
3Department of Engineering Dartmouth College, Hannover, New Hampshire , Plastic and Reconstructive Surgery, Weill Cornell Medical College, Houston Texas
*Corresponding Author : Joseph F Buell
Tulane University, New Orleans, Louisiana
Tel: 504-988-0783
Fax: 504-988-7510
E-mail: Jbuell1@tulane.edu
Received: October 25, 2017 Accepted: November 10, 2017 Published: November 17, 2017
Citation: Witt JG, Haugh AM, Adam Hauch MD, Darden M, Parker G, et al. (2017) Amniotic Membrane for the Treatment of Burns. J Plast Surg Cosmetol 1:1.
Abstract
The concept of using amniotic membrane for skin replacement is not new. The first documented use of fetal membranes during skin transplantation was performed in 1910. Three years later, Sabella and Stem applied amniotic membrane to burn patients. This initial use of amnion for burned skin demonstrated the clinical effectiveness of amniotic membrane, including: 1) increased re-epithelialization and healing as well as 2) decreased infection rates and pain. After decades of evolution in burn treatments, innumerable technologies have been developed, ranging from meshed autographs, AlloDerm�??, cultured skin, constructed biologic dermal matrix, and most recently, 3D laser printing. While these technologies are promising, they often pose significant therapeutic challenges, such as limited epithelialization, incomplete tissue incorporation, or excessive cost. These limitations present an opportunity to re-examine the potential therapeutic application of amniotic membrane in burn care.
Keywords: Amniotic membrane; Burn coverage; Cost analysis
Introduction
Recent developments in tissue procurement, screening, and banking have given rise to the use of biologic materials in a multitude of surgical procedures. The true salutary effects of biologic materials have been linked to the presence of innumerable cytokines, growth factors, and stem cells, previously unrecognized and underappreciated. Amniotic membrane currently has a multitude of applications, including burns, nerve regeneration, soft tissue reconstructive surgeries, ocular surgeries, and diabetic foot ulcers [1-3]. The use of amniotic membrane for second- and third-degree burns has been evaluated in a limited number of studies, as well as an unpublished clinical trial, completed in 2014, that compared amnion as a skin substitute to standard burn treatments [4]. A second similar clinical trial is currently recruiting in the United States, but most studies have been limited to developing countries. The majority of the studies presented in this review were therefore conducted in developing countries, which often have limited resources and a high incidence of burn-related trauma. This lends to the relevance and even potential benefits of amniotic membrane for burn care in institutions or environments that lack the resources necessary to provide traditional burn and wound care, which is both expensive and complicated. Conversely, procurement, processing and application of amniotic membrane is easily accessible, technically simple, and cost-effective. Amniotic membrane has been shown to increase healing rates, decrease rates of infection, shorten hospital stays, and decrease the number of dressing changes required in burn patients and thus has tremendous potential to improve outcomes and decrease cost. The effectiveness of amniotic membrane has been demonstrated in chronic wounds, such as diabetic foot ulcers, and shows great promise for the treatment of donor skin graft sites, wounds treated with skin grafts, and as a dressing for partial thickness burns (Table 1).
| Study | Design | Outcome Variables | Significant Results for Amnion Group |
|---|---|---|---|
| Branski et al., [15] | Randomized controlled trial-amniotic membrane compared to standard wound care for partial-thickness burns in pediatric patients which did not require skin grafts (n=102) | Length of hospital stay, rate of infection, time to total healing, frequency of dressing changes | Decreased dressing changes (p<0.05) |
| Adly et al., [11] | Randomized controlled trial- amniotic membrane compared to polyurethane membrane for skin graft donor sites in burn patients (n=46) |
Rates of infection, electrolyte distribution, serum albumin loss, incidence of pain, healing time frequency, frequency of dressing change | decreased rate of infection (p=0.047) decreased electrolyte losses (P=0.033) decreased serum albumin loss (P=0.033) decreased pain during dressing changes(p=0.023) decreased frequency of dressing changes (p=0.000) |
| Mostaque et al., [17] | Randomized prospective study-amniotic membrane compared to topical silver sulfadiazine for the treatment of partial-thickness burns not requiring skin grafts in children (n=102) | Number of days in hospital, number of dressing changes, time needed for epithelialization, expression and activity of children, pain and comfort between and during dressing changes, patient and guardian acceptance of treatment, opinions of attending doctor toward treatment | Decreased time for re-epithelialization of superficial (P<0.001) and deep second degree burn (P<0.001), decreased hospital stay time (P<0.05), decreased number of dressing changes (P<0.05), decreased pain during dressing changes (P<0.001) and between (P<0.001), patients remained more active (P<0.001), well accepted by patients and guardians (P<0.01), and attending felt more comfortable applying AM than SD (P<0.001) |
| Mohammadi et al., [13] | Prospective clinical trial- amniotic membrane compared to standard wound care for chronic burn wounds treated with skin allografts in symmetric extremity burns (n=76 limbs, 38 patients) |
Duration rate of graft take 21 days post application | Shortened duration of graft take (P<0.001) |
| Mohammadi et al., [14] | Prospective clinical trial- amniotic membrane compared to standard wound care for burn wounds treated with skin allografts in symmetric extremity burns (n=108 limbs, 54 patients) |
Duration rate of graft take 21 days post application | Shortened duration of graft take (P<0.001) |
| Salehi et al., 2013 [12] | Prospective Randomized control trial-amniotic membrane compared to standard wound care for the treatment of skin graft donor site on burn patients (n=42) |
Patient tolerance of wound dressing changes, duration of wound healing (re-epithelialization), wound site infection | Patient cooperation during wound dressing changes improved (P<0.000) and duration of wound healing decreased (P<0.000) |
| Eskandarlou et al., [18] | Clinical trial-amniotic membrane compared to standard wound care for skin graft donor site on burn patients (n=32) |
Severity of pain, movement, and risk of local infection | Improved movement from post-op day 1 to 5 (p=0.01), decreased pain from post-op day 1 to 3 (p=0.01) |
Table 1: Studies evaluating amniotic membrane for burn patient treatment used in this review.
Amniotic membrane
The amnion forms during the second week of embryonic development, soon after blastocyst implantation [5]. The amniotic membrane lines the innermost layer of the placenta, consisting of both amnion and chorion. It is composed of multiple layers, with various mesenchymal cells, and an epithelial layer closest to the embryo [1].
Amniotic membrane has several unique properties that contribute to the tissue’s ability to promote healing and reepithelialization. Studies have demonstrated that amnion and amniotic membrane products contain growth factors such as platelet derived growth factor AA (PDGF-AA), PDGF-B, epidermal growth factor (EGF), placental growth factor (PLGF), transforming growth factor α (TGF-α), TGFB1, basic fibroblast growth factor (bFGF), and granulocyte colony stimulating factor (GCSF), all of which are implicated in healing and regeneration [6]. Amniotic membrane has also been shown to up-regulate the synthesis of growth factors in culture [7]. Some of the growth factors that amniotic tissue contains also promote angiogenesis, a process that has been demonstrated with the implantation of amniotic tissue into the subcutaneous tissue of mice [8].
In addition to providing important growth factors, amnion has been shown to recruit stem cells to sites of healing and increase stem cell proliferation [9]. Amniotic tissue also contains anti-inflammatory cytokines such as IL-4, IL-6, IL-8, IL-10 and tissue inhibitor of metalloproteinase (TMP) 1, 2 and 4. The tissue and its derivative products contain lysozymes and immunoglobulins that also make it antibacterial.
A major benefit to amniotic products, especially when compared with other skin substitutes, is that they are generally nonimmunogenic. Amniotic epithelial cells have been found to lack HLA-A,B, C, or DR antigens and beta-2 microglobulin and have also been shown to decrease cytokine synthesis and the inflammatory response in vitro [10].
Methods
This study was conducted in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRIMSA-P) guidelines.
Selection criteria
Data from seven randomized controlled trials and one case series were included in this systematic review. All eight articles are from peer-reviewed English language journals and examine the effects of amniotic membrane on partial-thickness burns, donor skin graft sites, and burns treated with skin grafts. All publications were limited to the use of human subjects only.
Literature search strategy
Electronic searches were performed using Pubmed, Cochrane Central Register of Controlled Trials (CCTR), and Cochrane Database of Systematic Reviews (CDSR). The following keywords were used: “amnion,” “amniotic membrane,” and “burn.”
Date extraction
Two investigators reviewed each retrieved article to determine its relevance to this review. Discrepancies were eliminated by discussion between the reviewers and final results were reviewed by a senior investigator.
Discussion
Donor site healing rates
Amniotic membrane has been used to improve wound healing in a multitude of burn studies. This technology has shown significant capacity to regenerate burn surfaces as well as donor sites used to cover the burned area. With the varying severity and sizes of burns, the extent of unburned tissue used for donor skin grafts can be limited. This fact frequently complicates wound care and can lead to delayed burn coverage, increasing the risk and rate of wound infections and other secondary complications.
Adly et al. reported on the use of amniotic membrane for the coverage of skin graft donor sites in burn patients. This group was compared to skin graft site coverage with polyurethane membrane. Amniotic membrane led to improved wound healing, decreased electrolyte disturbance (P=0.033), lower serum albumin losses (P=0.033) and a lower incidence of infections (P=0.047) [11].
Other studies have examined the effectiveness of amniotic membrane as biologic dressings for donor sites in more extensive burn patients where skin was harvested to cover larger second- and third-degree burns on other areas. Salehi et al. identified that the time to healing for donor sites dressed with amniotic membrane was significantly shorter than those treated with standard burn care (P<0.001) [12]. This data concurred with the Adly study where amniotic membrane led to a 47.8% healing rate in the first 20 postoperative days compared to 39.1% for the polyurethane membrane dressing group [11]. Both authors attribute the improvement in wound healing to amnion’s composition of growth factors, antibacterial properties, and global decrease in immunogenicity and alloreactivity.
Burn allograft coverage
While the benefits to donor site healing are well-established, multiple other studies have examined the ability of amniotic membrane to improve burn coverage and healing compared to those treated with standard meshed skin grafts. Mohammadi et al. evaluated the efficacy of amniotic membrane as a secondary barrier for extremity burns. Burns debrided and grafted with donor skin grafts and secured with skin staples were compared to skin grafts covered with amniotic membrane. This study demonstrated the time to graft take for burns covered with amniotic membrane was significantly shorter than those secured with staples (P<0.001) [13]. Mohammedi et al. subsequently confirmed similar improvements in graft take when amniotic membrane was used in chronic burn wounds. Grafts covered with amnion were compared to those treated with standard of care in chronic burn wound patients and the time to graft take was found to be significantly shorter in skin grafts treated with amnion when compared with with standard of care (P<0.001) [14]. Burn wounds covered with granulation tissue are frequently associated with poor graft take and wound healing. Mohammedi et al. postulated that the antibacterial molecules found in amniotic tissue are able to penetrate granulate tissue and eliminate sources of breeding bacteria, therefore decreasing the complications seen in chronic wounds. Similar clinical findings have been observed after the application of liquid amnion to meshed skin grafts.
The efficacy of amniotic membrane in both acute and chronic granulating wounds is a critical observation. Despite the evolution of multiple new technologies and burn platforms, there are innumerable patients who, either through regional isolation or financial means, will not be able to access this level of care. This being said, it is all too uncommon for patients in developing countries to not immediately seek treatment for burns, leading to granulation and infection. Therefore, immediate or delayed use of amniotic membrane can improve subsequent graft take or wound healing for those patients suffering from acute or chronic burn wounds [14]. This same novel property could be exploited in innumerable military wounds, including blast and burn injuries that require prolonged extrication and evacuation often necessary during transfer to a definitive treating center.
Diminished dressing changes
Amnion tremendously improves patient’s quality of life. Pain is the greatest clinical challenge associated with burns, particularly in partial-thickness burns. The standard of care for these partialthickness burns is multi-faceted, with frequent topical medication applications and dressing changes, varying from two to four times a day. These dressing changes are often extremely painful, requiring high dose narcotics or even general anesthesia. Branski et al. compared a single application of amniotic membrane for partialthickness burns to standard burn dressings. Burn patients treated with amniotic membrane frequently required significantly fewer dressing changes than patients treated with standard of care alone (p<0.01) [15]. A similar study conducted by Bujang-Safawi et al. also evaluated a single application of amniotic membrane for partial thickness burn patients and found that over 85% of patients required only one application of the amnion membrane dressing [16].
This finding was consistent with the donor site data reported by Adly et al. that identified a significant decrease in dressing changes in amniotic membrane patients compared to those with polyurethane membrane dressings. In this study, only 30.4% of patients treated with amniotic membrane required more than one dressing change daily compared to 60.9% of patients treated with other non-biologic membranes. Some of these non-biologic membrane patients required as many as five dressing changes a day (P=0.001) [11]. As an indicator of clinical success and improved quality of life, Salehi et al. demonstrated that patients treated with amniotic tissue were significantly more cooperative in dressing changes compared to standard wound care changes (P<0.001) for donor graft sites [12].
Dramatic clinical improvements were observed when amniotic membrane was compared to silver sulfadiazine. Mostaque et al. evaluated the use of amniotic membrane for the treatment of partialthickness burns in children compared to silver sulfadiazine. Significant improvements in quality of life were identified in the amniotic membrane group. The use of amniotic membrane was associated with fewer days spent in the hospital (P<0.01), decreased dressing changes (P<0.01), and increased rates of re-epithelialization in both standard (P<0.001) and deep second-degree burns (P<0.001) [17].
Pain management
Multiple studies have suggested significant improvements in quality of life with the use of amniotic membrane, including increased compliance and more rapid discharge. Eskandarlou et al. focused on patient’s pain scores for donor graft sites treated with amniotic membrane dressings. Amniotic membrane patients had significantly less pain during the first three days following burn surgery compared with standard wound dressing. The study attributed the reduction in pain with the amnion membrane dressing to a moister environment, and the capability for quicker healing and re-epithelialization. As a secondary benefit, patients who had amniotic membrane applied to their donor sites regained significantly greater limb movement in the first five post-surgical days compared to those treated with standard wound dressing (p=0.01) [18].
All three donor graft studies confirmed the benefits of amniotic membrane in pain control. Salehi et al. documented higher pain scores reported by patients during dressing changes in patients treated with conventional wound dressings. His study attributed this to amnion creating a moister environment compared to standard care, allowing for easier dressing change [12]. Bujang-Safawi et al. reported that none of the patients treated with amniotic membrane for partial-thickness burns complained of pain [16]. Adly et al. found that 56.6% of patients treated with amniotic membrane did not report pain during dressing changes compared to 60.9% of patients treated with a polyurethane membrane (P=0.023) [11].
The ability for amniotic membrane to decrease dressing changes and reduce patient’s pain creates a significant benefit for burn patients. The improvements in quality of life include the potential for decreased severe anxiety before dressing changes, a common experience for many burn patients undergoing standard wound dressing changes [19]. Therefore, a decreased necessity for dressing changes can contribute to the patient’s improved quality of mental health and potentially improve the patient’s mobility, motivation, and overall outcome.
Cost analysis
Each year nearly 19,000 patients will experience a flame or chemical burn in the United States. The cost of treating a burn varies with the degree and extent of the burn itself. In 2010, moderate size burns were anticipated to cost an average $206,853 to treat compared to $1,617,345 in severe or extensive burns. Complicated burn patients have been reported to reach a total cost of greater than $10 million. Treatment costs of burns are quickly dwarfed when one considers the impact of productive years lost. These estimates of cost to society reached nearly $8.6 billion in 2011.
The average length of severe burn injuries is 75 days with the greatest initial burn care expense associated with burn unit beds (20%), dressings (15%), blood products (16%) and medications (17%). Complications impacting global costs include delayed wound closure, infections, fragile or failed skin grafts, wound contractures and psychological trauma. Amniotic membrane appears to impact these potential complications by decreasing wound infections, improving graft take, decreasing dressing changes and wound care pain, and shortening hospital stays.
Conclusion
Amniotic membrane is a biologic material with historic use in several settings that has recently been rediscovered for the treatment of burn patients. Acute and chronic burns are equally responsive to the membrane due to the antibacterial agents and and human growth factors found in amniotic membrane and amniotic membrane derived products. Amniotic membrane immediately epithelializes a burn injury without posing a risk of metalloprotein accumulation or alloreactivity. Amniotic membrane is safe and efficacious and its use in several studies has demonstrated significant improvements in clinical outcomes as well as quality of life for partial and full thickness burn patients. Our analysis suggests that, especially considering our modern understanding of biologics, membrane should be adopted as standard of care for burn patients.
References
- Fairbairn NG, Randolph MA, Redmond RW (2014) The clinical applications of human amnion in plastic surgery. J Plast Reconstr Aesthetic Surg JPRAS 67: 662-675
- Bhattacharya N, Stubblefield P (2010) Regenerative Medicine Using Pregnancy-Specific Biological Substances. Springer Sci & Business Media
- Arora R, Mehta D, Jain V (2005) Amniotic membrane transplantation in acute chemical burns. Eye Lond Engl 19: 273-278.
- Study of Donated Amnion, Fetal Placental Membrane, as Skin Substitute for Burn Patients (2016) ClinicalTrials.gov
- Moore K L, Persaud TVN, Torchia MG (2011) The Developing Human: Clinically Oriented Embryology with Student Consult Online Access, 9th Edition
- Koob TJ (2013) Biological properties of dehydrated human amnion/chorion composite graft: implications for chronic wound healing. Int Wound J 10: 493-500
- Koob TJ, Lim JJ, Massee M, Zabek N, Denozière G (2014) Properties of dehydrated human amnion/chorion composite grafts: Implications for wound repair and soft tissue regeneration. J Biomed Mater Res B Appl Biomater 102: 1353-1362.
- Koob TJ (2014) Angiogenic properties of dehydrated human amnion/chorion allografts: therapeutic potential for soft tissue repair and regeneration. Vasc Cell 6: 10
- Massee M (2015) Dehydrated human amnion/chorion membrane regulates stem cell activity in vitro. J Biomed Mater Res B Appl Biomater.
- Akle CA, Adinolf M, Welsh K I, Leibowitz S, McCol I (1981) Immunogenicity of human amniotic epithelial cells after transplantation into volunteers. Lancet Lond Engl 2: 1003-1005.
- Adly O A (2010) Assessment of amniotic and polyurethane membrane dressings in the treatment of burns. Burns J Int Soc Burn Inj 36: 70-710.
- Salehi SH , As AK, Mousavi SJ, Shoar S (2015) Evaluation of Amniotic Membrane Effectiveness in Skin Graft Donor Site Dressing in Burn Patients. Indian J Surg 77: 427-431.
- Mohammadi AA , Johari H G, Eskandari S (2013) Effect of amniotic membrane on graft take in extremity burns. Burns J Int Soc Burn Inj 39: 1137-1141.
- Mohammadi AA (2013) Effect of fresh human amniotic membrane dressing on graft take in patients with chronic burn wounds compared with conventional methods. Burns J Int Soc Burn Inj 39: 349-353.
- Branski LK (2008) Amnion in the treatment of pediatric partial-thickness facial burns. Burns J Int Soc Burn Inj 34: 390-399.
- Bujang SE, Halim AS, Khoo TL, Dorai AA (2010) Dried irradiated human amniotic membrane as a biological dressing for facial burns a 7-year case series. Burns J Int Soc Burn Inj 36: 876-882.
- Mostaque AK, Rahman KB (2011) Comparisons of the effects of biological membrane (amnion) and silver sulfadiazine in the management of burn wounds in children. J Burn Care Res Off Publ Am Burn Assoc 32: 200-209.
- Eskandarlou M, Azimi M, Rabiee S, Seif RMA (2016) The Healing Effect of Amniotic Membrane in Burn Patients. World J Plast Surg 5: 39-44.
- The Impact of Stress at Dressing Change in Patients With Burns: A Review of the Literature on Pain and Itching (2016) Wounds.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi