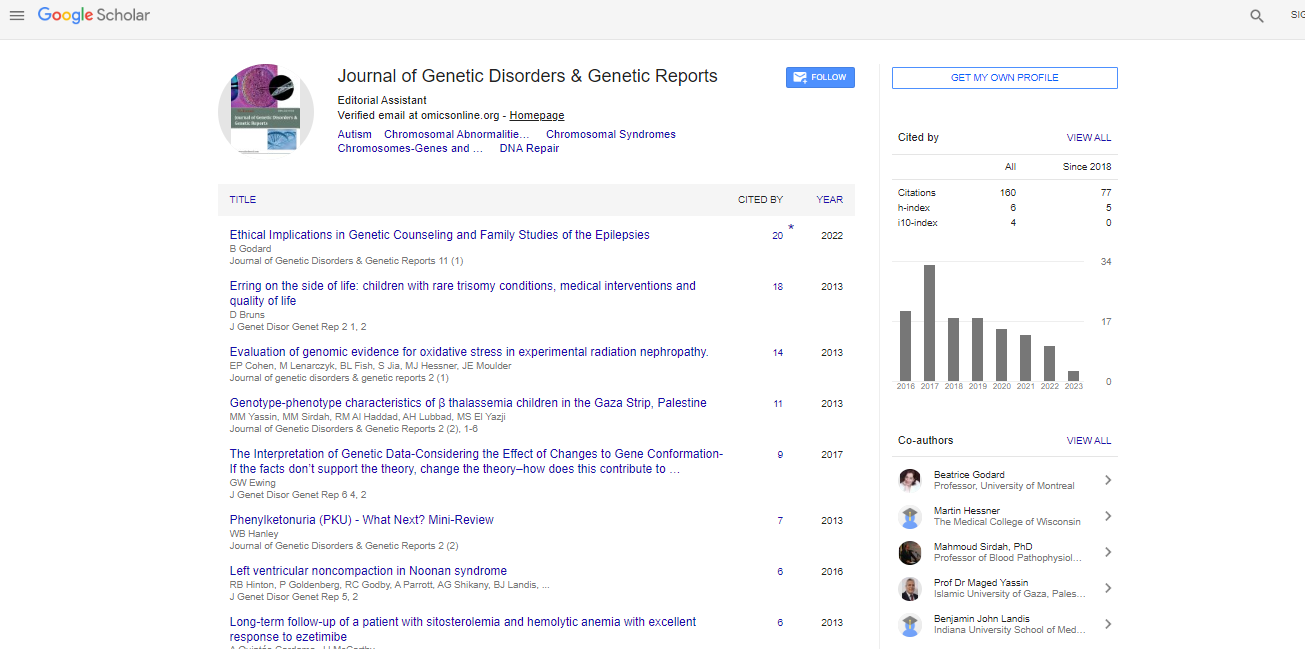
Review Article, J Genet Disor Genet Rep Vol: 7 Issue: 2
Advances of Programmed Death-1/Programmed Death-1 Ligand Signal Pathway and its Blockers in Nasopharyngeal Carcinoma
Zhou Q, Assani G, Ling H, Xiong Y and Zhou Y*
Department of Radiation and Medical Oncology, Hubei Key Laboratory of Tumor Biological Behaviors, Zhongnan Hospital of Wuhan University, Wuhan, Hubei Province, PR China
*Corresponding Author : Zhou Y
Department of Radiation and Medical Oncology, Hubei Key Laboratory of Tumor Biological Behaviors, Zhongnan Hospital of Wuhan University, Wuhan, Hubei Province, PR China
Tel: +(861) 3907154247
E-mail: yfzhouwhu@163.com
Received: June 25, 2018 Accepted: August 03, 2018 Published: August 14, 2018
Citation: Zhou Q, Assani G, Ling H, Xiong Y, Zhou Y (2018) Advances of Programmed Death-1/Programmed Death-1 Ligand Signal Pathway and its Blockers in Nasopharyngeal Carcinoma. J Genet Disor Genet Rep 7:2. doi: 10.4172/2327-5790.1000176
Abstract
Nasopharyngeal carcinoma is one of the most common malignancies of head and neck squamous cell carcinoma in southern China and is closely related to Epstein-Barr virus infection. Although the treatment efficacy of nasopharyngeal carcinoma has been made an obvious progress during the recent years, there are still some patients suffering from relapse or metastasis, which remains a difficult condition to manage. Recently, immunotherapy targeting programmed death-1/programmed death-1 ligand signal pathway has made a remarkable breakthrough in the treatment of many solid tumors including head and neck squamous cell carcinoma, which could be a new treatment after surgery, radiotherapy, chemotherapy and targeted therapy. Even though lots of clinical trials targeting programmed death-1/programmed death-1 ligand signal pathway have been carried out, the value of anti-programmed death-1/programmed death-1 ligand immunotherapy in nasopharyngeal carcinoma is not yet clear. This review aims to summarize recent advances in the clinical research of programmed death-1/programmed death-1 ligand signal pathway and their blockers in nasopharyngeal carcinoma.
Keywords: Nasopharyngeal carcinoma; PD-1; PD-L1; EBV; Immunotherapy
Introduction
Nasopharyngeal carcinoma (NPC) is characterized by Epstein-Barr virus (EBV) infection and high prevalence in South China, Southeast Asia, the Arctic and North Africa areas, while is rare in western countries [1]. Along with the development of precise radiotherapy technologies and combined chemotherapies, the treatment efficacy of NPC has been made an obvious progress during the recent years. Unfortunately, there are still about 10% of patients with local recurrence and 20% with distant metastasis [2,3]. Among them, patients with distant metastases have a median survival of only 19-21 months [4]. Based on these issues, high-efficient and novel treatments are needed to improve survival.
Substantial tumor-infiltrating lymphocytes (TILs) are widely considered to be an indicator of immune interaction between host and tumor and are implicated in NPC. Generally, the appearance of TILs is a favorable prognostic factor in many cancers, since it shows that the tumor is recognized by the immune system and can therefore be cleared by cytotoxic T cells. However, tolerogenic immune suppression such as rich population of T regulatory cells (Tregs) amongst TILs can contribute to the functional inactivation of cytotoxic T cell responses, which plays an important role in oncogenesis and development of NPC. Anti-immunosuppressive therapies have developed rapidly in recent years, especially in the signal pathway of anti- programmed death-1/programmed death-1 ligand (PD-1/PD-L1). PD-L1 is involved in the induction of Tregs suggesting that activation of PD-L1 could, via Tregs proliferation, result to tumor immunosuppression and immune escape whereas its blocking could enhance the endogenous anti-tumor effects. As reported by clinical trials of anti-PD-1 and anti-PD-L1 antibodies, many solid tumors such as non-small cell lung cancer (NSCLC) [5], renal cell carcinoma [6], bladder cancer [7] and breast cancer [8] have all showed good efficacy and relatively low adverse reactions. Based on the positive results of these clinical trials, two anti- PD-1 antibodies and three anti-PD-L1 antibodies have been successively approved by American Food and Drug Administration (FDA) for the treatment of certain kind advanced malignant tumors. However, more have to know about PD-1/PD-L1 signal pathway in NPC because the clinical value of PD-1 and PD-L1 in NPC is not yet clear. This review aims to summarize recent advances in the clinical research concerning the relation between PD-1 and PD-L1, their blockers and the blockers applications in NPC, for providing more information about the application of PD1 and PD-L1 blockers in basic research and clinical test of NPC, especially for the patients with local recurrence or distant metastasis.
EBV and Host Immunity in NPC
EBV, also known as Human Herpesvirus 4 (HHV-4), is the first DNA virus found related to human tumors, which spreads primarily through saliva to infect lymphoid tissue B cells. In the healthy hosts, the invading EBV enters the "latency phase" without any clinical symptoms under normal immune system surveillance, while in immunocompromised hosts, EBV proliferates vigorously in lymphoid tissues and lead to host immunity disorders [9]. The regulation of host immune system by EBV is closely related to the occurrence and development of various human tumors, including gastric cancer, lung cancer, breast cancer, nasopharyngeal carcinoma and Hodgkin's lymphoma.
NPC is a multi-gene hereditary malignancy in the nasopharyngeal area with significant regional differences and ethnic aggregation [1]. EBV infection, heredity, and environmental factors [10] are now considered to be implicated in mutation of genes involved in occurrence and development of NPC. EBV-associated NPC tumor cells typically express the latent membrane proteins 1(LMP1), latent membrane proteins 2A(LMP2A), latent membrane proteins 2B (LMP2B), EBV nuclear antigen 1 (EBNA1) and several EBV noncoding RNAs (EBERs) [11]. Among them, LMP1 is the most important EBV-encoded tumorigenic protein involved in cell transformation, cell apoptosis, cell differentiation, cell cycle, and participates in the invasion and metastasis of malignant tumors [12].
Apart from the crucial role of EBV and immune escape ability in the development of NPC, its relationship between immune checkpoints PD-1/PD-L1 has also been reported by many researchers. A recent study [13] found that PD-L1 expression level was positively related to LMP1 in EBV positive NPC cell lines both exogenous overexpression and endogenous induction of LMP1 could result in significant increase of PD-L1 expression. Further study found that the up-regulation of PD-L1 mediated by LMP1 was related to several key pathways, such as STAT3, AP-1, and NF-κ B, which stimulate PD-1/PD-L1 signal pathway activation and eventually leading to immune escape. Such previously undiscovered novel function of LMP1 may provide new direction into the tumorigenesis and development of EBV-driven NPC.
PD-1/PD-L1 Signal Pathway
Structure and expression of PD-1
Also known as CD279, PD-1 is a type I transmembrane glycoprotein inhibitory receptor that was firstly acquired from apoptotic T cell hybridomas by Ishida [14] in 1992 via the use of the subtractive hybridization technique. PD-1 is a member of the immunoglobulin B7-CD28 subfamily and consists of extracellular domain, hydrophobic transmembrane domain and cytoplasmic domain. With the immunoreceptor tyrosine-based inhibitory motif (ITIM) at its proximal membrane end and the immunoreceptor tyrosine-based switch motif (ITSM) at its distal membrane end of cytoplasmic domain, these two tyrosine residues are implicated in execution of PD-1 function [14], which is closely related to effector T cell immune response and mediation of immune escape. PD-1 is known as mainly expressed in various immune cells, including activated CD4+ T cells, CD8+ T cells, B cells, natural killer T cells, monocytes and dendritic cells [15]. In addition, it is reported that PD-1 is expressed on the surface of Tregs, which promotes Tregs proliferation and strengthens the inhibitory immune response [16].
Structure and expression of PD-1 ligands
Also called B7-H1 or CD274, and B7-DC or CD273 respectively, PD-L1 and PD-L2 are currently the only two known PD-1 ligands. Like PD-1, PD-L1 and PD-L2 are type I transmembrane glycoproteins composed of extracellular domain, hydrophobic transmembrane domain and cytoplasmic domain. On the molecular structure, PD-L1 and PD-L2 possess 40% identical amino acid sequence. PD-L1 is highly expressed in a variety of human malignant tumor cells, such as melanoma, renal cell carcinoma, multiple myeloma, breast cancer, bladder cancer, colon cancer, and lung cancer [17]. Besides, PD-L1 is also reported to be expressed in tumor infiltrating dendritic cells, tumor infiltrating lymphocytes and tumor infiltrating macrophages [18,19]. Compared with PD-L1, PD-L2 possesses a more limited distribution which is only expressed on the membrane surface of macrophages, dendritic cells and some B-cell subsets with a low expression level [20].
Interaction between PD-1 and PD-1 ligands
It has been confirmed that the affinity between PD-1 and its ligands was different. Compared with the interaction between PD-L1 and PD-1, the combination of PD-L2 andPD-1 possesses a 2~6-fold higher affinity and shows a different association and dissociation kinetics. Assume that PD-L1 and PD-L2 are expressed at the same level, PD-L1 would not able to outcompete PD-L2 for binding PD-1. However, extremely limited distribution and generally more lower expression of PD-L2 confirm the binding ability of PD-L1 as the primary binding ligand of PD-1. That could also be the reason of the low role of PD-L2 in modulating tumor immunity. Moreover, PD-L1 has a preferential role in regulating Type 1 T helper immune response (Th1 response), whereas PD-L2 may regulate Type 2 T helper immune response (Th2 response) [20].
PD-L1 binds not only to PD-1, but also binds to CD-80 (B7-1) on the surface of activated T cells to transmit negative regulatory signals [21]. Although the anti-PD-1 and anti-PD-L1 antibodies act together on the PD-1 and PD-L1 signal axis, a single type blocker could not block this signal pathway completely. Because PD-1 blockers could only prevent the binding of PD-1 to PD-L1 and PD-L2, but it could not block the interaction of PD-L1 and CD80. Likewise, anti-PD-L1 antibody can stop the binding of PD-L1 to PD-1 and CD-80 but could not prevent the interaction of PD-1 and PD-L2. Therefore, some researchers suggest that the combination of anti-PD-1 antibodies with anti-PD-L1 antibodies would deliver better clinical results than monotherapy [22]. However, until now there is no conclusive evidence favoring such positive results in clinical trials. It will be good to encourage many studies concerning PD-1 and PD-L1 complementary antibodies in NPC to assess their possible additional effect or possible adverse effects and toxicities.
Mechanism of PD-1/PD-L1 inhibitory signal pathway
The human immune system eliminates tumor cells through T-cell immune responses by recognizing tumor-specific antigens and tumorassociated antigens. Complete activation of T cells requires three signals (Figure 1) [23], Signal 1 is the T cell receptor (TCR) signal which recognized the antigenic peptide-major histocompatibility complex (p-MHC) presented by antigen-presenting cells (APCs) that activate tyrosine kinases including ZAP70. Signal 2 is the binding of co-stimulatory molecules such as CD28, in which mostly PI3 kinase is activated. Signal 3 is the cytokine receptor signals, in which most cytokines, including interleukins, IFNs, and hematopoietic growth factors, activate the Janus kinase (JAK)/signal transducer and activator of transcription (STAT) pathway [24]. The microenvironmental regulation of T cells can be described as a fourth or modulating signal for T-cell activation and function [25].
Figure 1: T-cell immune responses and PD-1/PD-L1 inhibitory signal pathway [23].
The link of PD-1 and its ligands together to the TCR signal, leads to the cytoplasmic domain tyrosine ITSM phosphorylation and then recruiting of SRC Homology 2-Domain-Containingprotein Tyrosine Phosphatase 1 (SHP-1), which in turn dephosphorylates several key molecules on the TCR signal pathway, such as Zap70 and PI3K.The dephosphorylation of these key molecules promotes their inactivation, inhibition of downstream signal, and eventually induce CD8+T and CD4+T cell anergy (Figure 1). Nevertheless, the specific mechanisms of T cell anergy have not been fully understood but may include induction of T cell tolerance, T cell apoptosis, T cell depletion, enhanced Tregs cell function and inducible co-stimulatory molecules (ICOS) and PD-1 imbalance.
There are three major T cell activation signals, signal 1, signal 2 and signal 3. Signal 1 is MHC-antigen-peptide complex-TCR signal that activate tyrosine kinases including ZAP70. Signal 2 is the costimulatory signals from CD28, in which mostly PI3 kinase is involved. Signal 3 is the cytokine receptor signals that activate the JAK/STAT pathway. T cell activation by TCR, co-simulators, and cytokines is blocked by (1) PD-1, (2) CTLA4, and (3) SOCS.
Clinical Significance of PD-1 and PD-L1 in NPC
Prognosis value of PD-L1
Most retrospective analysis indicated that NPC tumor cells highly express PD-L1 (Table 1), with a positive expression rate from 89% to 100% [26-31]. The patients with high PD-L1 expression level possess a worse prognosis than that with low PD-L1 expression [26-29]. Similar results have been reported in malignant melanoma [32] and renal cell carcinoma [33]. In contrast, Lee [34] found that only 25% of NPC tumor cells express PD-L1 and high expression of PD-L1 means better local recurrence free survival (LRFS) and disease free survival (DFS). This opposite result is also found in lung squamous cell carcinoma [35] and breast cancer [36]. However, a larger sample size study [37] reported that the expression of PD-L1 in NPC tumor cells (TC) (24%) was much lower than that in TILs (75%) with a cutoff value of 1%, and without any relation with the prognostic parameter such as overall survival (OS) and progress free survival (PFS). A previous small sample study by Hus et al. [30] also showed that PD-L1 expression level in NPC tumor cells was not associated with patients’ outcome (Table 1).
| Author (Year) | Patients | PD-L1% | Cutoff value | Clinical Correlation | Prognosis |
|---|---|---|---|---|---|
| Han X (2017) [26] | 65 | 89% TC | ≥ 5% TC | PC: PD-1 | poor PFS |
| 65 | 58% TC | ≥ 10%TC | unrelated | poor PFS OS | |
| Zhou Y (2017) [27] | 99 | 97% TC | positively stained | NC: BMI, HB | poor OS |
| Zhou Y (2017) [28] | 132 | 97% TC | positively stained | NC: rT classification, HB | poor OS |
| Zhang J (2015) [29] | 139 | 95% TC | >5% stained cells | —— | poor DFS |
| Hsu MC (2010) [30] | 28 | 100% TC | —— | unrelated | unrelated |
| Chen BJ (2013) [31] | 18 | 89% TC | > 5% TC | —— | —— |
| Lee VH (2016) [34] | 104 | 25% TC | ≥ 5% TC | unrelated | better LRFS DFS |
| Chan OS (2017) [37] | 161 | 76%(75%TILs, 24%TC) | ≥ 1% TILs or TC | unrelated | unrelated |
| 161 | 24%(17%TILs, 15%TC) | ≥ 5% TILs or TC | unrelated | unrelated |
Table 1: Results from clinical researches of PD-L1 in NPC.
Taken together, it can be considered that PD-L1 is highly expressed in NPC, and its high expression may indicate poor prognosis. However, there are several studies with controversial results as of prognostic significance, which may due to the differences of sample size, baseline, treatment options and tumor heterogeneity. Moreover, several studies indicated that the detectable PD-L1 expression level is largely susceptible to antibodies, test methods, scoring standards, and positive cutoff values. Another problem that we cannot avoid is that when we suppose to detect PD-L1 expression, shall we detect the tumor parenchymal cells alone or take tumor stromal cells and immune cells simultaneously? According to the existed clinical trials, the default generic detection schema is partial to base on PD-L1 staining both on TC and TILs with a cutoff value of 1% by immunohistochemistry (IHC). But this is not a recognized gold standard. Only when the above problems are solved, the value of PDL1 expression level in the prognosis of NPC patients can be determined.
PD-L1 with clinicopathological characteristics
With regard to the relationship between PD-L1 expression and clinicopathological characteristics in NPC, the majority of present studies [26,31,34,37] agreed that there is no correlation between PD-L1 and the patient's age, gender, smoking, staging, and histological type. Otherwise, it is found in a retrospective study of 132 recurrent NPC patients [28] that high expression of PD-L1 was significantly associated with rT classification of recurrent tumors. They also [27,28] suggested that the expression of PD-L1 was negatively correlated with plasma hemoglobin (HB) content and body mass index (BMI), but not with the peripheral blood EBV DNA load and PD-1 expression, which is inconsistent with previous founding [38-40] where the expression of PD-L1 in EBV-associated malignant tumors can be upregulated by EBV-encoded LMP1. One possible explanation is that the EBV DNA load in circulating plasma may be an inactive residue of EBV infection in the previous active period, which results to an inaccurate detection of EBV DNA load and its correlation with PD-L1. Perhaps a more sensitive method of detecting present EBV DNA load can eliminate this interference so that we can replace the detection of PD-L1 by indirectly detecting EBV viral load to guide the treatment of PD-1/PDL1 checkpoint blockade in NPC.
According to a study [26] with stage IVa, when the PD-L1 positive threshold was set to at 5%, there was an obviously positive correlation between PD-L1 and PD-1 expression on tumor cells, but when the positive threshold was set to at 10%, only a correlation trend was observed between PD-L1 and PD-1 expression (Table 1). It is speculated that there is an interaction between PD-1 and PD-L1 expression in tumor cells. As reported in the study of Kleffel [32], the PD-1 pathway in tumor cells can be activated by the tumor cells’ own PD-L1 and eventually leading to tumor progression. The high level of PD-L1 is associated with anemia suggesting that hypoxia may induce immune deficiency through the PD-1/PD-L1 axis [41], but its specific mechanism is still unclear and needs further investigation.
Prognosis and clinicopathological characteristics of PD-1
Previous studies [27-30] have suggested that PD-1 is only expressed on the surface of NPC immune cells, and the expression rate of PD-1 is lower than that of PD-L1 by about 30%-40%. However, report of Han [26] where it is found for the first time that PD-1 is also expressed on the surface of NPC tumor cells with corresponding expression rates (88% and 38% separately) when the positive threshold is set at 5% and 10% respectively (Table 2). Similar study has also been reported in melanoma [32], which suggests that the expression of PD-1 and PD-L1 and their mechanisms of interaction is more complicated than what we have found in current studies.
| Author (Year) | Patients | PD-1% | Cutoff Value | Clinical Correlation | Prognosis |
|---|---|---|---|---|---|
| Han X (2017) [25] | 65 65 |
88% TC 38% TC |
≥ 5% TC ≥ 10%TC |
unrelated unrelated |
unrelated unrelated |
| Zhou Y (2017) [26] | 99 | 44.4% TILs | positively stained | unrelated | unrelated |
| Zhou Y (2017) [27] | 132 | 37.9% TILs | positively stained | unrelated | unrelated |
| Zhang J (2015) [28] | 139 | 37.4% TILs | H-score>0 | —— | poor DFS (PD-1/PD-L1 co-expression) |
| Ooft ML (2017) [42] | 78 | 76% | >40/field(200×) | —— | better OS (PD-1/PD-L1 co-expression) |
| Hsu MC (2010) [29] | 46 46 |
28.4% CD8+T 15.6 % CD4+T |
positively stained positively stained |
unrelated unrelated |
poor OS, DFS, LRFS unrelated |
Table 2: Results from clinical researches of PD-1 in NPC.
Although there aren’t any relation between PD-1 expression status in NPC and patients’ clinicopathological characteristics, its relationship with prognosis remains controversial. Multiple studies [26-28] have reported that PD-1 is not associated with the prognosis of NPC patients. While a small sample research [30] found that patients with PD-1 positive expression had a shorter OS, DFS, and LRFS, which means a worse prognosis. However, Zhang [29] reported that a single expression of PD-1 is not an independent prognostic factor for NPC, but co-expression of PD-1 and PD-L1 may reflect a significant reduction in DFS (Table 2). In contrast, a study by Ooft [42] found that co-expression of PD-1 and PD-L1 may predict a better OS. Nevertheless, all these studies above have the problems of small sample size short follow-up time and less incidents of recurrence or metastasis. Therefore, further studies are required by using more large-sample multi-center prospective researches for great confirmation.
Based on the fact that the use of PD-1, PD-L1, and their coexpression as prognostic indicators of advanced NPC has not been discovered yet, the clinical significance of immunotherapy targeting PD-1/PD-L1 in NPC is not much clear. However, as reported from the current published clinical trials, both anti-PD-1 antibodies and anti- PD-L1 antibodies have appeared good efficacy and low adverse reactions in many advanced tumors, which suggesting that PD-1/PDL1 blockers might be equally effective in advanced NPC.
Clinical Trial of Anti-PD-1/PD-L1 Therapy in NPC
PD-1/PD-L1 immune checkpoint blockers
Recently, the anti-PD-1 monoclonal antibodies mainly include Opdivo (Nivolumab), Keytruda (Pembrolizumab) and Pidilizumab (CT-011). Anti-PD-L1 monoclonal antibodies mainly include BMS-936559 (MDX1105), Tecentriq (Atezolizumab or MPDL3280A), Durvalumab (MEDI4736) and Avelumab (MSB0010718C). Among them, the PD-1 inhibitors Keytruda and Opdivo have been approved by the American Food and Drug Administration (FDA). The former is applicable to patients with advanced or unresectable melanoma who are no longer responding to other medications, and the latter has also been approved for the treatment of metastatic squamous NSCLC that continues to progress after chemotherapy and classical Hodgkin's lymphoma that relapses or progresses after treatment. In 2016, the FDA approved the first PD-L1 inhibitor, Tecentriq, for the treatment of locally advanced or metastatic urothelial carcinoma. Then, in 2017, Imfinzi (Durvalumab) and Bavencio (Avelumab) were approved successively by the FDA. The former has the similar indications as Tecentriq, and the latter is the first treatment for metastatic Merkel cell carcinoma in adolescents over 12 years of age.
Current clinical trials of anti-PD-1/PD-L1 treatment in NPC
As of Jun 10, 2018, according to the information obtained from PubMed and Clinicaltrials.gov website, there are only two clinical trials concerning Pembrolizumab and Nivolumab in NPC. In the nonrandomized- multicohort, phase Ib clinical trial KEYNOTE-028 (NCT02054806) [43], the 27 recurrent or metastatic nasopharyngeal carcinoma (RM-NPC) patients with PD-L1 positive expression received a dose of 10 mg/kg Pembrolizumab treatment every 2 weeks up to 2 years or until disease progression or unacceptable toxicity. The results revealed that the objective response rate (ORR) and duration of response (DOR) reached 25.9% and 17.1 months, respectively. Despite of these encouraging results, most PD-L1 positive patients did not respond to pembrolizumab treatment. Since this study did not include PD-L1-negative patients for comparison and their sample size are limited, it will be difficult to conclude that PD-L1 positive is a potential effective biological indicator for anti-PD-1 antibody therapy. In another multicenter phase II clinical trial (NCT02339558) (n=43) [44], it was observed that PD-L1 positive RM-NPC patients may be more likely to benefit from Nivolumab than PD-L1 negative expression. However, according to certain clinical trials of NSCLC [45,46] part of PD-L1-negative NSCLC patients could also benefit from anti-PD-1 and anti-PD-L1 therapy, and there is no significant correlation between PD-L1 status and ORR[46]. These data suggest that the use of PD-L1-positive only as an effective biological indicator for anti- PD-1/PD-L1 therapy can exclude potential immunotherapy-benefiting patients. Although both two trials showed that drugs targeting PD-1 have achieved a certain efficacy and low toxicity in the treatment of RM-NPC patients, more researches with high grade evidence are needed to know more concerning its therapeutic effect.
In advanced NPC, the phase II clinical trial pembrolizumab (NCT02611960) is currently underway where the recruitment criteria is RM-NPC patients who have undergone platinum chemotherapy, regardless of PD-L1 expression status. It is believed that the results of this trial will help to evaluate the predictive effect of PD-L1 in anti- PD-1 treatment on RM-NPC. Besides, the strategies for detection of laboratory indicators for selection of the dominant population for anti- PD-1/PD-L1 treatment in NPC remains to discover. Based on the existed clinical studies, it could be suggested that explore the relevance of certain marker such as peripheral blood Epstein-Barr virus DNA loadHB content and other candidate indicators will be good for enhancement of treatment efficacy. However, the efficacy of anti- PD-1/PD-L1 therapy in patients with locally advanced non-RM-NPC has not been studied at present, which might be a new direction for the researchers in the future.
Future perspectives
PD-1/PD-L1 immune checkpoint blockers have shown rapid onset, long-lasting response and good tolerability in many solid tumors, hematological malignancies, and have appeared inspiring efficacy in RM-NPC. However, from clinical trials to clinical applications, there are such problems which need to be resolved and further confirmed. The predictive treatment value of PD-L1 for anti-PD-1/PD-L1 immunotherapy on NPC is not yet clear. Then, how to select the dominant population to individualize and optimize treatment has becoming the most important issue at present. Moreover, exploring different treatment modalities in NPC must be study such as administration in single dose or combined administration (combined with chemotherapy, radiation, or other targeted drugs). Much have to know about the timing of administration, first-line, second-line, or third-line. Whether there is a more effective and less toxic immune checkpoint inhibitor except PD-1/PD-L1.
Nowadays, PD-L1 remains to be the most widely studied biomarker in prediction the efficacy of anti-PD-1/PD-L1 immunotherapy, but it was also thought [47,48] that it exists other markers, such as inflammatory factors and tumor-related genes, which may predict the efficacy of pembrolizumab immunotherapy. Recently, immune checkpoint blockers combined with chemotherapy have progressed toward first-line treatment of some malignant tumors. For example, the ORR of carboplatin combined with pembrolizumab in advanced NSCLC was significantly higher than that of chemotherapy alone (55% vs 29%) [49]. In addition, new immune checkpoint inhibitors have also been estimating in clinical trials, such as lymphocyte activation gene 3 (LAG3) monoclonal antibody (NCT01968109) and killer cell immunoglobulin-like receptors (KIRs) monoclonal antibodies. The combination of different immune checkpoint inhibitors can fully activate innate and adaptive immunity and screen out the optimum combination to achieve the best effectiveness. For instance, two studies [50,51] indicated that anti-PD-1 or PD-L1 antibodies combined with anti-LAG3 or IL-2 shows better therapeutic effects. The combined administration of anti-PD-1 antibody and anti-PD-L1 antibody has also been reported to have better efficacy than single use in preclinical models [52].
Conclusion
NPC is one of the EBV infected and TILs associated malignancies with a very limited treatment for patients with local recurrence or distal metastasis. The NPC patients’ PD-L1 expression status was positively correlated with rT classification and PD-1 expression, and negatively correlated with HB, BMI and peripheral blood EBV DNA load. The NPC patients with high expression of PD-1PD-L1 or their co-expression have a poor prognosis due to the activation of PD-1/PDL1 signal pathway while more researches with high grade evidence are still needed to confirmed this correlation. Moreover, the perturbation of PD-1/PD-L1 functional axis by using anti-PD-1 monoclonal antibodies have shown encouraging results in clinical trials for PD-L1 positive RM-NPC patients.
Generally, immunotherapy targeting PD-1/PD-L1 signal pathway as a new treatment for NPC patients with local recurrence or distal metastasis could improve the prognosis of RM-NPC patients. But more fundamental and clinical researchers have to encouraged for assessing and confirmation of the link between PD-1 and PD-L1, prognosis value of the PD-1/PD-L1 axis and the efficacy of the use of its blockers alone or in association to another treatment such as radiotherapy, chemotherapy and target therapy.
Acknowledgements
The authors would like to thank all the doctors of Department of Chemoradiotherapy of Zhongnan Hospital for their supports.
References
- Yu MC, Yuan JM (2002) Epidemiology of nasopharyngeal carcinoma. Semin Cancer Biol 12: 421-429.
- Sun X, Su S, Chen C, Han F, Zhao C, et al. (2014) Long-term outcomes of intensity-modulated radiotherapy for 868 patients with nasopharyngeal carcinoma: an analysis of survival and treatment toxicities. Radiother Oncol 110: 398-403.
- Li AC, Xiao WW, Shen GZ, Wang L, Xu AA, et al. (2015) Distant metastasis risk and patterns of nasopharyngeal carcinoma in the era of IMRT: long-term results and benefits of chemotherapy. Oncotarget 6: 24511-24521.
- Jin Y, Shi YX, Cai XY, Xia XY, Cai YC, et al. (2012) Comparison of five cisplatin-based regimens frequently used as the first-line protocols in metastatic nasopharyngeal carcinoma. J Cancer Res Clin Oncol 138: 1717-1725.
- Fehrenbacher L, Spira A, Ballinger M, Kowanetz M, Vansteenkiste J, et al. (2016) Atezolizumab versus docetaxel for patients with previously treated non-small-cell lung cancer (POPLAR): a multicentre, open-label, phase 2 randomised controlled trial. Lancet 387: 1837-1846.
- McDermott DF, Sosman JA, Sznol M, Massard C, Gordon MS, et al. (2016) Atezolizumab, an anti-programmed death-ligand 1 antibody, in metastatic renal cell carcinoma: long-term safety, clinical activity, and immune correlates from a phase Ia study. J Clin Oncol 34: 833-842.
- Rosenberg JE, Hoffman-Censits J, Powles T, van der Heijden MS, Balar AV, et al. (2016) Atezolizumab in patients with locally advanced and metastatic urothelial carcinoma who have progressed following treatment with platinum-based chemotherapy: a single-arm, multicentre, phase 2 trial. Lancet 387: 1909-1920.
- Nanda R, Chow LQ, Dees EC, Berger R, Gupta S, et al. (2016) Pembrolizumab in patients with advanced triple-negative breast cancer: phase Ib KEYNOTE-012 study. J Clin Oncol 34: 2460-2467.
- Sabeti M, Kermani V, Sabeti S, Simon (2012) JH Significance of human cytomegalovirus and Epstein-Barr virus in inducing cytokine expression in periapical lesions. Journal of Endodontics 38: 47-50.
- Chua MLK, Wee JTS, Hui EP, Chan ATC (2016) Nasopharyngeal carcinoma. Lancet 387: 1012-1024.
- Hao SP, Tsang NM, Chang KP (2004) Monitoring tumor recurrence with nasopharyngeal swab and latent membrane protein-1 and epstein-barr nuclear antigen-1 gene detection in treated patients with nasopharyngeal carcinoma. Laryngoscope 114: 2027-2030.
- Ersing I, Bernhardt K, Gewurz BE (2013) NF-κB and IRF7 pathway activation by epstein-barr virus latent membrane protein 1. Viruses 5: 1587-1606.
- Fang W, Zhang J, Hong S, Zhan J, Chen N, et al. (2014) EBV-driven LMP1 and IFN-γ up-regulate PD-L1 in nasopharyngeal carcinoma: implications for oncotargeted therapy. Oncotarget 5: 12189-12202.
- Ishida Y, Agata Y, Shibahara K, Honji T (1992) Induced expression of PD-1, a novel member of the immunoglobulin gene superfamily, upon programmed cell death. EMBO J 11: 3887-3895.
- Keir ME, Butte MJ, Freeman GJ, Sharpe AH (2008) PD-1 and its ligands in tolerance and immunity. Annu Rev Immunol 26: 677-704.
- Francisco LM, Salinas VH, Brown KE, Vanguri VK, Freeman GJ, et al. (2009) PD-L1 regulates the development, maintenance, and function of induced regulatory T cells. J Exp Med 206: 3015-3029.
- Obeid JM, Erdag G, Smolkin ME, Deacon DH, Patterson JW, et al. (2016) PD-L1, PD-L2 and PD-1 expression in metastatic melanoma: correlation with tumor-infiltrating immune cells and clinical outcome. Oncoimmunology 5: e1235107.
- Mu CY, Huang JA, Chen Y, Chen C, Zhang XG (2011) High expression of PD-L1 in lung cancer may contribute to poor prognosis and tumor cells immune escape through suppressing tumor infiltrating dendritic cells maturation. Med Oncol 28: 682-688.
- Taube JM, Klein AP, Brahmer JR, Xu H, Pan X, et al. (2014) Association of PD-1, PD-1 ligands, and other features of the tumor immune microenvironment with response to anti-PD-1 therapy. Clin Cancer Res 20: 5064-5074.
- Ghiotto M, Gauthier L, Serriari N, Pastor S, Truneh A, et al. (2010) PD-L1 and PD-L2 differ in their molecular mechanisms of interaction with PD-1. Int Immunol 22: 651-660.
- Butte MJ, Keir ME, Phamduy TB, Sharpe AH, Freeman GJ (2007) Programmed death-1 ligand 1 interacts specifically with the B7-1 costimulatory molecule to inhibit T cell responses. Immunity 27: 111-122.
- Topalian SL, Drake CG, Pardoll DM (2012) Targeting the PD-1/B7-H1(PD-L1) pathway to activate anti-tumor immunity. Curr Opin Immunol 24: 207-212.
- Chikuma S, Kanamori M, Mise�Omata S, Yoshimura A (2017) Suppressors of cytokine signaling: Potential immune checkpoint molecules for cancer immunotherapy. Cancer Sci 108: 574-580.
- O’Shea JJ, Gadina M, Schreiber RD (2002) Cytokine signaling in 2002: new surprises in the Jak/Stat pathway. Cell 109: S121-131.
- Samstag Y, John I, Wabnitz, GH (2013) Cofilin: a redox sensitive mediator of actin dynamics during T-cell activation and migration. Immunol Rev 256: 30-47.
- Han X, Huang L, Li WT, Wang RZ (2017) Expression of PD-1 and PD-L1 in patients with stage IVa nasopharyngeal carcinoma and its clinical significance. Clin J Radiat Oncol 26: 1131-1136.
- Zhou Y, Shi D, Miao J, Wu H, Chen J, et al. (2017) PD-L1 predicts poor prognosis for nasopharyngeal carcinoma irrespective of PD-1 and EBV-DNA load. Sci Rep 7: 43627.
- Zhou Y, Shi D, Wu H, Tang H, Kuang J, et al. (2017) PD-1 and PD-L1 expression in 132 recurrent nasopharyngeal carcinoma: the correlation with anemia and outcomes. Oncotarget 8: 51210-51223.
- Zhang J, Fang W, Qin T, Yang Y, Hong S, et al. (2015) Co-expression of PD-1 and PD-L1 predicts poor outcome in nasopharyngeal carcinoma. Med Oncol 32: 86.
- Hsu MC, Hsiao JR, Chang KC, Wu YH, Su IJ, et al. (2010) Increase of programmed death-1-expressing intratumoral CD8 T cells predicts a poor prognosis for nasopharyngeal carcinoma. Mod Pathol 23: 1393-1403.
- Chen BJ, Chapuy B, Ouyang J, Sun HH, Roemer MG, et al. (2013) PD-L1 expression is characteristic of a subset of aggressive B-cell lymphomas and virus-associated malignancies. Clin Cancer Res 19: 3462-3473.
- Kleffel S, Posch C, Barthel SR, Mueller H, Schlapbach C, et al. (2015) Melanoma cell-intrinsic PD-1 receptor functions promote tumor growth. Cell 162: 1242-1256.
- Xu, F, Xu L, Wang Q, An G, Feng G, (2015) Clinicopathological and prognostic value of programmed death ligand-1 (PD-L1) in renal cell carcinoma: a meta-analysis. Int J Clin Exp Med 8: 14595-14603.
- Lee VH, Lo AW, Leung CY, Shek WH, Kwong DL, et al. (2016) Correlation of PD-L1 expression of tumor cells with survival outcomes after radical intensity-modulated radiation therapy for non-metastatic nasopharyngeal carcinoma. Plos One 11: e0157969.
- Schmidt LH, Kümmel A, Görlich D, Mohr M, Bröckling S, et al. (2015) PD-1 and PD-L1 expression in NSCLC indicate a favorable prognosis in defined subgroups. Plos One 10: e136023.
- Baptista MZ, Sarian LO, Derchain SF, Pinto GA, Vassallo J (2016) Prognostic significance of PD-L1 and PD-L2 in breast cancer. Hum Pathol 47: 78-84.
- Chan OS, Kowanetz M, Ng WT, Koeppen H, Chan LK, et al. (2017) Characterization of PD-L1 expression and immune cell infiltration in nasopharyngeal cancer. Oral Oncol 67: 52-60.
- Li Z, Lai Y, Sun L, Zhang X, Liu R, et al. (2016) PD-L1 expression is associated with massive lymphocyte infiltration and histology in gastric cancer. Hum Pathol 5: 182-189.
- Fang W, Hong S, Chen N, He X, Zhan J, et al. (2015) PD-L1 is remarkably over-expressed in EBV-associated pulmonary lymphoepithelioma-like carcinoma and related to poor disease-free survival. Oncotarget 6: 33019-33032.
- Paydas S, Bagir E, Seydaoglu G, Ercolak V, Ergin M (2015) Programmed death-1 (PD-1), programmed death-ligand 1 (PD-L1), and EBV-encoded RNA (EBER) expression in Hodgkin lymphoma. Ann Hematol 94: 1545-1552.
- Barsoum IB, Smallwood CA, Siemens DR, Graham CH (2014) A mechanism of hypoxia-mediated escape from adaptive immunity in cancer cells. Cancer Res 74: 665-674.
- Ooft ML, van Ipenburg JA, Braunius WW, Zuur CI, Koljenovi�?�? S, et al. (2017) Prognostic role of tumor infiltrating lymphocytes in EBV positive and EBV negative nasopharyngeal carcinoma. Oral Oncol 71: 16-25.
- Hsu C, Lee SH, Ejadi S, Even C, Cohen RB, et al. (2017) Safety and antitumor activity of pembrolizumab in patients with programmed death-ligand 1-positive nasopharyngeal carcinoma: results of the KEYNOTE-028 study. J Clin Oncol 35: 4050-4056.
- Ma BB, Goh BC, Lim WT (2017) Multicenter phase II study of nivolumab in previously treated patients with recurrent and metastatic non-keratinizing nasopharyngeal carcinoma—Mayo Clinic Phase 2 Consortium P2C-MN026, NCI9742, NCT02339558. Cancer Res 77: CT076.
- Grosso JF, Horak CE, Inzunza HD (2013) Association of tumor PD-L1 expression and immune biomarkers with clinical activity in patients (pts) with advanced solid tumors treated with nivolumab (anti-PD-1; BMS-936558; ONO-4538). J Clin Oncol 31: 3016.
- Antonia SJ, Grosso JF, Horak CE: Association of tumor PD-L1 expression and immune biomarkers with clinical activity in patients with non-small cell lung cancer (NSCLC) treated with nivolumab (Anti-PD-1; BMS-936558; ONO-4538). WCLC 2013:11-35.
- Muro K, Chung HC, Shankaran V, Geva R, Catenacci D, et al. (2016) Pembrolizumab for patients with PD-L1-positive advanced gastric cancer (KEYNOTE-012): a multicentre, open-label, phase 1b trial. Lancet Oncol 17: 717-726.
- Seiwert TY, Burtness B, Mehra R, Weiss J, Berger R, et al. (2016) Safety and clinical activity of pembrolizumab for treatment of recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-012): an open-label, multicentre, phase 1b trial. Lancet Oncol 17: 956-965.
- Langer CJ, Gadgeel SM, Borghaei H, Papadimitrakopoulou VA, Patnaik A, et al. (2016) Carboplatin and pemetrexed with or without pembrolizumab for advanced, non-squamous non-small cell lung cancer: A randomised, phase 2 cohort of the open-label KEYNOTE-021 study. Lancet Oncol 17: 1497-1508.
- West EE, Jin HT, Rasheed AU, Penaloza-Macmaster P, Ha SJ, et al. (2013) PD-L1 blockade synergizes with IL-2 therapy in reinvigorating exhausted T cells. J Clin Invest 123: 2604-2615.
- Goding SR, Wilson KA, Xie Y, Harris KM, Baxi A, et al. (2013) Restoring immune function of tumor specific CD4+ T cells during recurrence of melanoma. J Immunol 190: 4899-4909.
- Curran MA, Montalvo W, Yagita H, Allison JP. (2010) PD-1 and CTLA-4 combination blockade expands infiltrating T cells and reduces regulatory T and myeloid cells within B16 melanoma tumors. Proc Natl Acad Sci USA 107: 4275-4280.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi