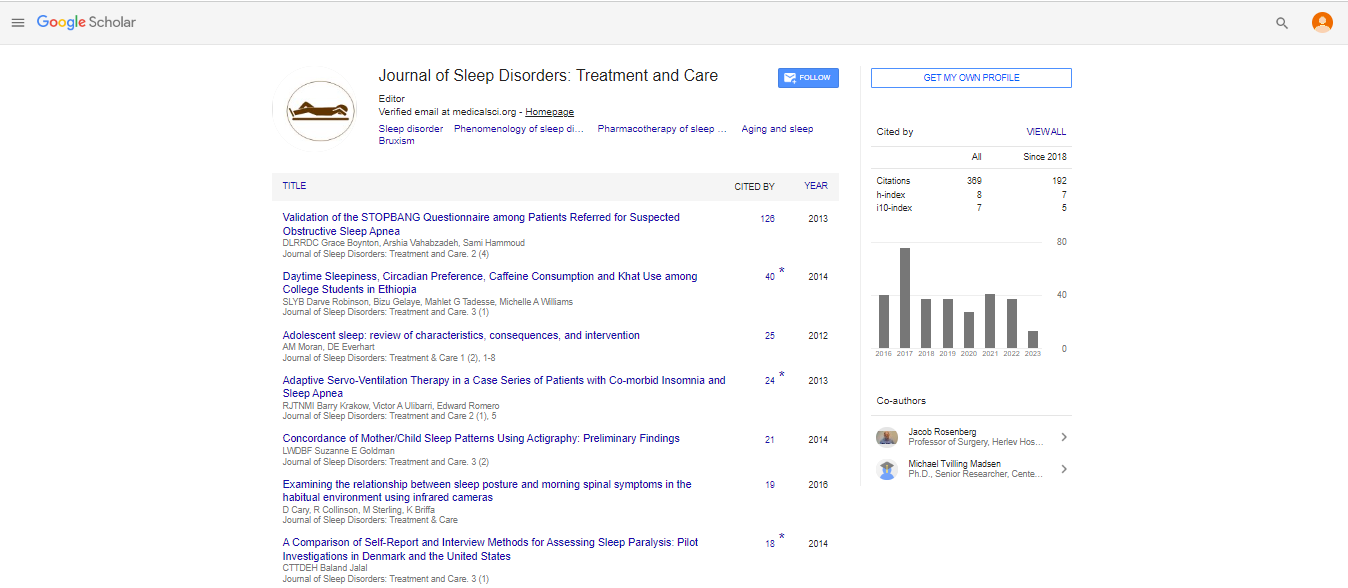
Review Article, J Sleep Disor Treat Care Vol: 10 Issue: 6
Activity in Patient with Epileptiform RBD Like Symptomatology
Jane Jessica*
Department of Microbiology, Osmania University,Hyderabad, India
*Corresponding Author: Jane Jessica
Department of Microbiology, Osmania University,Hyderabad, India
E-mail: jessicaj1995@gmail.com
Received: June 03, 2021 Accepted: June 17, 2021 Published: June 24, 2021
Citation: Jane J, 2021, Activity in Patient with Epileptiform RBD Like Symptomatology. J Sleep Disor: Treat Care , 10:6. (277)
Abstract
RBD is a parasomnia with behavioral pattern frequently associated with synucleinopathies. It can emulate central epileptic seizures, fundamentally front facing and transient flap seizures. These clinical similitudes among RBD and nighttime epileptic seizures may result in misdiagnosis. The hyperkinetic engine appearances revealed in front facing epileptic seizures can be suggestive of the energetic and savage arm and leg developments seen in RBD. Engine and verbal automatisms related with transient projection seizures may emulate the motioning and somniloquy observed in RBD. A few examinations show that epilepsy and RBD may exist together, however this data is scant .
Keywords: parasomnia
Introduction
RBD is a parasomnia with behavioral pattern frequently associated with synucleinopathies. It can emulate central epileptic seizures, fundamentally front facing and transient flap seizures. These clinical similitudes among RBD and nighttime epileptic seizures may result in misdiagnosis. The hyperkinetic engine appearances revealed in front facing epileptic seizures can be suggestive of the energetic and savage arm and leg developments seen in RBD. Engine and verbal automatisms related with transient projection seizures may emulate the motioning and somniloquy observed in RBD. A few examinations show that epilepsy and RBD may exist together, however this data is scant .
Discussion
We portray a patient with PD and meningiomas with unusual rest practices that happened during NREM feelings of excitement related with successive epileptiform movement. PD has customarily been viewed as an engine framework problem, however it is currently generally perceived to be a perplexing issue with assorted clinical highlights that incorporate rest aggravations [6]. Rest grievances in these patients incorporate a sleeping disorder, daytime languor with rest assaults, anxious legs condition and rest authorization practices, similar to the ones announced by our patient [7]. Rest sanctioning practices in PD and other synucleinopathies are all the more much of the time brought about by RBD. This problem is described by dream-sanctioning conduct that generally shows as battling practices and bad dreams and happens during REM rest, related with the deficiency of the ordinary REM rest related atonia. As of late, be that as it may, other rest practices named "Excitement Related Motor Behavioral Episodes (AMBES)" have been portrayed in these gathering of patients, but at lower frequencies than RBD. They can show as ordinary NREM parasomnias looking like sleepwalking or confusional feelings of excitement [8] and furthermore developments that happen during brief feelings of excitement both in REM and NREM rest [9,10]. Epilepsy is quite possibly the main differential determinations in parasomnias. Regardless of the way that it must be avoided for RBD analysis as per current rules [11] most investigations so far have centered in separating epilepsy from NREM parasomnias [12]. Not very many investigations have taken a gander at the affiliation or differential analysis among RBD and epilepsy [4,5]. Clinically, particularly in old patients with synucleinopathies, with non-cliché, strange rest related practices, some of the time related with dream content, epilepsy is infrequently suspected.
Conclusion
The primary clinical ramifications of this case is to bring issues to light for a potential job of epileptiform action in patients with RBD-like symptomatology and the need of neurophysiologic assessments even in patients where clinical thinking would obviously recommend a REM parasomnia. Making an analysis of epilepsy is an extraordinary occasion. Other than constant prescription changes, it carries other significant ramifications to regular daily existence. In our nation, for example, patients can't drive except if seizure free for one year. Moreover, there are as yet significant social shame related with this conclusion. Indeed, even in our patient, where PD related dementia had effectively caused the vast majority of these changes, the choice to add ongoing enemy of epileptic medications, with conceivable results and connections, to a generally poly-sedated old, ought to never be a simple one. Full v-PSG, with full EEG montages at whatever point the clinical doubt of epilepsy is high, ought to consistently be performed.
References
1. Bazil CW (2004) Nocturnal seizures. Seminars in Neurology 24: 293-300.
2. Schenck CH, Mahowald MW (2002) REM sleep behavior disorder: Clinical, developmental, and neuroscience perspectives 16 years after its formal identification in SLEEP. Sleep 25: 120-138.
3. D'Cruz OF, Vaughn BV (1997) Nocturnal seizures mimic REM behavior disorder. Am J End Technol 37: 258-264.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi