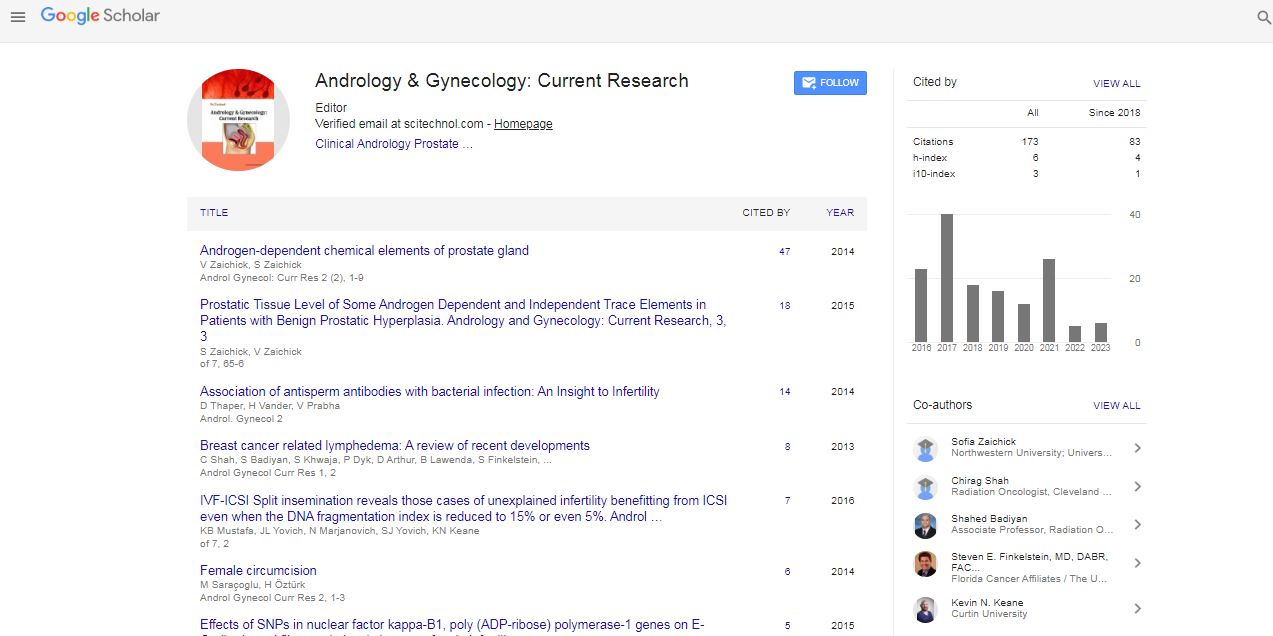
Research Article, Androl Gynecol Curr Res Vol: 6 Issue: 1
A Modified Technique for Performing Transurethral Nephroscopy Lithotripsy of Bladder Stones with/without Plasma Kinetic Resection of the Prostate of Benign Prostatic Hyperplasia: A New Bladder Stone Operation Method
Mao Shanhua1#, Ji Ying2#, Yin Qiuping2#, Zou Lujia1, Wang Lujia1, Li Guoqiang1, Wu Zhong1 and Gao Peng1*
1Department of Urology, Huashan Hospital, Fudan University, China
2Department of Nursing, Huashan Hospital, Fudan University, China
#These authors contributed equally to the work
*Corresponding Author : Gao Peng
Department of Urology, Huashan Hospital, Fudan University, Shanghai, China
Tel: +86 21 6564 2222
E-mail: hsurologygp@163.com
Received: January 31, 2018 Accepted: February 06, 2018 Published: February 13, 2018
Citation: Shanhua M, Ying J, Qiuping Y, Lujia Z, Lujia W, et al. (2018) A Modified Technique for Performing Transurethral Nephroscopy Lithotripsy of Bladder Stones with/without Plasma Kinetic Resection of the Prostate of Benign Prostatic Hyperplasia: A New Bladder Stone Operation Method. Androl Gynecol: Curr Res 6:1. doi: 10.4172/2327-4360.1000161
Abstract
Purpose: To probe the effective treatment for patients with Begin Prostate Hyperplasia (BPH) along with bladder stones with Plasmakinetic Resection of Prostate combining with Transurethral Nephrolithotripsy by Pneumatic and Ultrasound Lithotripsy´╝? Methods: Twenty five cases of patients of BPH combined with bladder stones were chosen. Plasmakinetic Resection of Prostate Combining with Transurethral Nephrolithotripsy by Pneumatic and Ultrasound Lithotripsy was used to compare the maximal urinary flow rate (Qmax), residual urine and other index in those patients before and after operations. Results: All operations in 25 cases were successful, without any complications. Three months after operations, Qmax, and residual urine were significantly improved in patients. Conclusions: Simultaneous transurethral bladder calculi lithotripsy combined with PKRP is considered as the safe, effective and minimal invasive surgical method to cure BPH along with bladder stones, also obviously improving the symptoms of obstruction, effectively removing calculus and improving the quality of life.
Keywords: Benign prostate hyperplasia; Bladder stone; PKRP
Introduction
Benign prostate hyperplasia (BPH) is quite common among the aged men. Frequent or urgent urination, increased nocturnal urination and endless urination caused by BPH bring great trouble to our patient’s daily life. If also complicated by bladder stones, they will be further bothered by more severe urinary irritation symptoms. Nowadays, bladder stones can be treated by extracorporeal shockwave lithotripsy (SWL), transurethral cystoscopy lithotripsy, percutaneous lithotripsy or bladder stonesotomy [1-4]. Among minimal-invasive choices, the efficiency of lithotripsy is comparatively low, while complications such as urethral stricture will happen on the contrary. In order to decrease the complications and increase the efficiency of lithotripsy, we applied percutaneous nephroscopy lithotripsy EMS equipment into transurethral lithotripsy and combined Plasma Kinetic Resection of the Prostate (PKRP) of BPH simultaneously. We have performed 25 cases of bladder stone patients with BPH by EMS transurethral nephroscopy lithotripsy (TUNL) and PKRP between June 2014 and December 2015. The present study aims to determine the safety and efficiency of the new combination treatment of BPH with bladder stone patients.
Materials and Methods
General information
We retrospectively collected the data of 25 cases of bladder stone with BPH male patients. Average age was 62.2 years old (54~82 y-o). All the patients presented with frequent or urgent urination, increased nocturnal urination, endless urination, hematuria, dysuria, even urinary retention. The study included 6 cases of bladder stones patients, 19 cases of bladder stones with BPH patients. Two patients got urethral stricture. Among 25 cases, eight patients got single stone and seventeen ones got multiple stones. The average total diameter of bladder stones was 2.6 CM (0.8~3.8CM). The peak flow and average flow of uroflometry were significantly decreased for all BPH patients.
Preoperative preparation
Before operations, routine urine and blood test, chemical test, immune test including prostate specific antigen (PSA), ultrasound, chest X-ray, Electrocardiogram, urine culture, X-ray (kidney-ureterbladder, KUB) and intravenous pyelography (IVP) were performed in all the patients. If urinary tract infection confirmed, suitable antibiotics would be taken according to the sensitiveness test. All of them got the urine white blood cell < 100/μL before operation. Transrectal prostate ultrasound, uroflometry, urodynamic examination were performed in 19 patients with BPH to make sure the diagnosis and exclude the Neurogenic bladder patients. Hypertension should be controlled under 150/90mmHg. Urethral catheter would be put for patients diagnosed as renal insufficiency (caused by bilateral hydronephrosis secondary to urinary obstruction) for 2~4 weeks until hydronephrosis and renal function recovered before operation.
Operation procedure
After general anesthesia or epidural anesthesia, lithotomy position was taken. Wolf F20 nephroscope with outer sheath was inserted into bladder visually through urethra with saline as rinse solution. The prostate and bladder were carefully observed, including the size and number of bladder stones and anatomic landmark of bilateral ureter orifices. EMS ultrasonic lithotripsy system was connected afterwards. For stones with high degree of hardness, pneumatic lithotripsy was first performed to split the stones into small pieces. Later, EMS ultrasonic lithotripsy system was applied to dust the stones and suck them out. On the contrary, EMS ultrasonic lithotripsy system was directly applied with no need of pneumatic lithotripsy. If patients complicated by BPH, PKRP was implemented afterward. At last, F22 silicone trifoveolate catheter was placed to rinse.
Postoperative treatment
Preventive anti-biotic treatment was prescribed for 2~3 days after operations for all patients. Nineteen BPH patients got continuous bladder irrigation for 1~2 days until the color of rinsing solution becoming clear. Urethral catheter was removed after 4~5 days, whereas, it should be kept at least 2~4 weeks if complicated by urethral stricture and urethral dilation implemented regularly.
Results
All the operations were satisfied. The average time of bladder stone lithoclasty and clearing was 30.1 minutes (15~55 minutes). The average time of PKRP was 40.2 minutes (35~55 minutes) with average amount of bleeding 70 mL (50~100 mL). No blood transfusion happened. No complications such as vesical perforation, TURP syndrome or severe infection occurred. KUB and ultrasound were performed after operation. Stone free rate was 100% with no residual stones. The length of hospitalization was 5~7 days. After catheter removed, urination symptoms of BPH patients got significantly improved. Among all 19 BPH patients, uroflometry was performed again during follow-up. Qmax (peak flow) reached 14~25 mL/s and average urinary flow rate 17 mL/s, which were significantly higher than data before operations. Residual urine test was also examined, which reached average 6.3 ± 3.2 mL, significantly better than preoperation status. No one got residual stones or recurrence of stones in 1~6 month’s postoperative follow-up (Figures 1a and 1b).
Discussion
BPH is a common disease among the elder, which is also the main cause of lower urinary obstructive disease. Lots of lower urinary tract syndromes (LUTS) such as frequent or urgent urination, increased nocturnal urination and endless urination occur because of BPH. What’s more increased residual urine volume or foreign body inside the bladder makes the stone formation becomes possible. A prospective study showed that 51% of patients presenting with bladder stones got the diagnosis of BPH [5,6]. In other words, approximately 10% of the BPH patients got complicated by bladder stones. With the booming development of micro-invasive urology, TURP replaces as the golden standard treatment of BPH, for the reason of minimal invasiveness, exact effectiveness and quick recovery. Whereas, PKRP is an even newer technique different from traditional TURP. In comparison, PKRP has the following characteristics [7,8]:
• Cutting under low temperature, energy penetrating superficially with regional loop
• No electricity current passing through the human body, so that effectively preventing the obturator nerve reflex
• Greatly reducing the injury of erectile nerve inside and outside the prostate capsule
• Using saline as irrigation fluid to prevent TURS
• Satisfied hemostatic effect and no need to fix the electrode plate onto human body.
For the treatment of bladder stones, open surgery is tending to be replaced by lots of intracavitary operations gradually, for instance, vigorously lithotrite lithotripsy, pneumatic lithotripsy, laser lithotripsy, ultrasonic lithotripsy etc. Different kinds of traditional intracavitary lithotripsy treatment share different advantages or disadvantages. By way of illustration, vigorously lithotrite lithotripsy is only suitable for stones <3.0 cm in diameter, meanwhile, it will also cause bleeding of prostate easily when we insert the lithotrite into a BPH patient with large middle lobe. What’s more, urethral stricture is also a common complication because of repeated in-andout procedure to remove the stone fragments. For holmium laser lithotripsy, it’s suitable for almost all hardness levels of stones, and capable of fragmenting urinary stones of all compositions, whereas lots of stone fragments floating inside the bladder cavity after lithotripsy, which will definitely influence the vision and therefore, the nurse is always busy to change the irrigation fluid bags to keep full supply [9]. Moreover, some small fragments are easily to move away in that situation, which might cause bladder perforation if laser aiming with errors. While for the large and multiple bladder stones, it’s quite slow to split and clear them. And the most important problem is that all the traditional lithotripsy can only split the stones while it’s impossible to discharge them at the same time. Swiss EMS ultrasonic pneumatic lithotripsy and stone clearing system combines pneumatic lithotripsy, ultrasonic lithotripsy and vacuum aspiration device altogether into one whole system. It’s able to aspirate and clear the stone fragments by vacuum pressure, which is the main advantage that differs with others. The design of the hollow ultrasonic probe with micro-hole anti-clogging structure can effectively reduce the heat generated, and greatly reduce the occurrence of probe channel obstruction. Therefore, the system is able to work for enough time and play a better performance on ultrasonic lithotripsy. Because of the instant vacuum aspiration, the vision is better than other lithotripsy methods, especially for multiple stones. The operating time has been tremendously shortened, while stone clearance rate per unit time has been greatly increased for various ingredients of the stone. In these years, we performed 25 cases of transurethral lithotripsy combined with pneumatic lithotripsy using nephroscope for bladder stones. Among them, all the stones were removed successfully within onetime completion. Comparatively shorter operating time, less bleeding volume and no severe complications made satisfactory results. To sum up, we found there are lots of advantages when using EMS to treat bladder stones:
• Stones were easily crushed into pieces and could be aspired at the same time, which resulted to short operation time and high stone free rate.
• The combination use of water irrigation inside and vacuum aspiration system outside kept the water flow circulating continuously. What’s more, clear vision would guarantee utmost operation continuity.
• There’s no need to insert the scope repeatedly, so that, the possibility of urethral injury decreased
• Using normal saline as irrigation water and vacuum aspiration system would be greatly free of TURS (transurethral resection syndrome) which caused by high bladder cavity pressure or water absorption.
• To conclude our experience, it’s better to pay attention to these four points:
• Well control of the irrigation velocity to fix the stone not to move too much and keeping the balance of water in and out can avoid the bladder mucosa injury or perforation and reduce the operation time.
• For patients complicated by BPH, the order of PKRP followed by bladder stone EMS operation can effectively reduce the possibility of ureter orifice injury caused by unclear vision of prostate cutting surface errhysis. Moreover, if PKRP first, it will lead to large volume of water absorption through the cutting surface.
• For bladder stones with diameter <2 cm, we use ultrasonic aspiration probe to crush the stones from the edge; while, for the stones with diameter >2 cm, the pneumatic lithotripsy probe should be first used to crush the large, and then, change to ultrasonic probe. During ultrasonic lithotripsy, the probe should be parallel to the scope operative channel; otherwise, even a small angle might lead to probe fractured. Among our 25 cases, no bladder perforation and water intoxication happened.
Conclusion
In summary, transurethral nephrolithotomy combined with PKRP for benign prostatic hyperplasia with bladder stones patients can remove the stones at one-time and relieve the lower urinary tract obstruction, with great clinical efficacy. The benefits such as little trauma, short operation time, easy to use, quick recovery, less pain is known and this method is worthy of being recommended.
Acknowledgment
This work was funded by grants from National Natural Science Foundation of China (Grant No. 81400705). and the National Basic Research Program of China (973 Program) (2015CB943003).
References
- Aron M, Agarwal MS, Goel A (2003) Comparison of percutaneous with transurethral bladder stonesotripsy in patients with large prostates and large vesical calculi undergoing simultaneous transurethral prostatectomy. BJU Int. 91: 293-295.
- Kilciler M, Sumer F, Bedir S, Ozgok Y, Erduran D (2002) Extracorporeal shock wave lithotripsy treatment in paraplegic patients with bladder stones. Int J Urol. 9: 632-634.
- Wollin TA, Singal RK, Whelan T, Dicecco R, Razvi HA, et al. (1999) Percutaneous suprapubic bladder stonesotripsy for treatment of large bladder calculi. J Endourol 13: 739-744.
- Barnes RW, Bergman RT, Worton E (1963) Litholapaxy vs. Bladder stonesotomy. J urol 89: 680-681.
- Yoshida T, Kinoshita H, Nakamoto T, Yanishi M, Sugi M, et al (2015) Conservative Treatment for Benign Prostatic Hyperplasia in Patients With Bladder Stones. Urology 86: 450-453.
- Millan-Rodriguez F, Errando-Smet C, Rousaud-Baron F, Izquierdo-Latorre F, Rousaud-Baron A, et al (2004) Urodynamic findings before and after noninvasive management of bladder calculi. BJU Int 93:1267-1270.
- Tu XA, Zhuang JT, Zhao L, Zhao LY, Zhao JQ, et al. (2013) Transurethral bipolar plasma kinetic resection of ejaculatory duct for treatment of ejaculatory duct obstruction. J Xray Sci Technol 21: 293-302.
- Kong CH, Ibrahim MF, Zainuddin ZMA (2009) Prospective, randomized clinical trial comparing bipolar plasma kinetic resection of the prostate versus conventional monopolar transurethral resection of the prostate in the treatment of benign prostatic hyperplasia. Ann Saudi Med 29: 429-432.
- Patel AP, Knudsen BE (2014) Optimizing use of the holmium: YAG laser for surgical management of urinary lithiasis. Curr Urol Rep 15: 397.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi