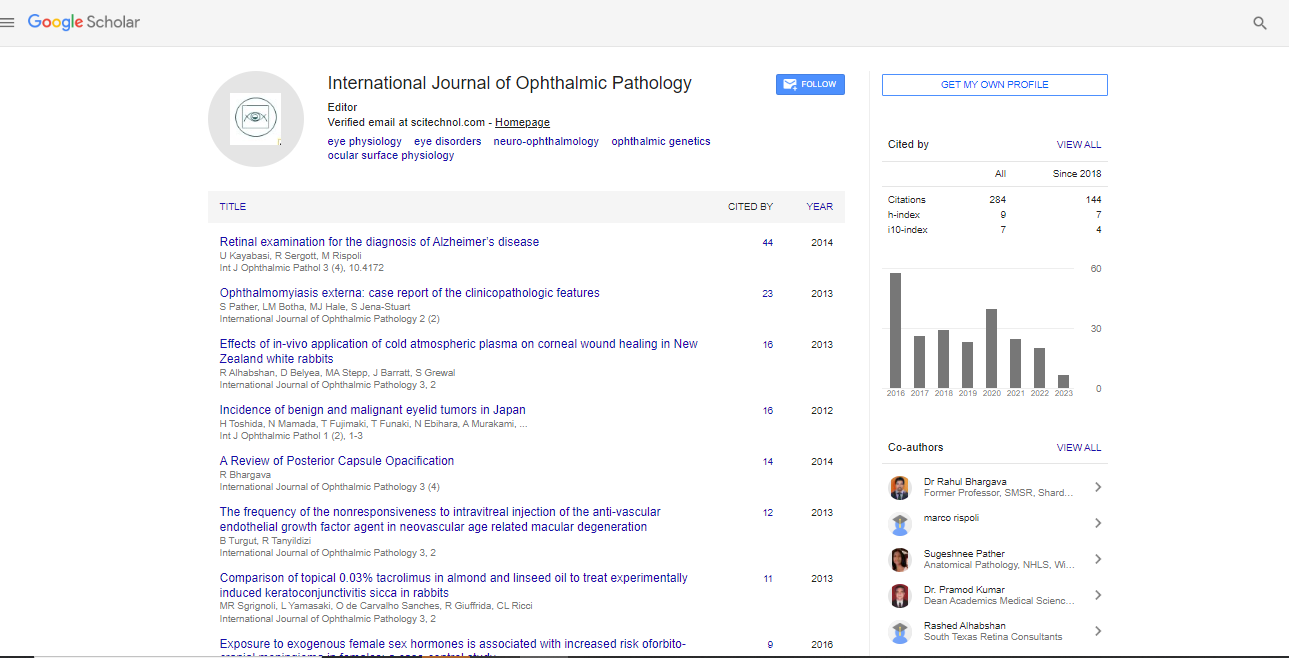
Clinical Image, Int J Ophthalmic Pathol Vol: 4 Issue: 3
A Description of the Pathological Features of Rheumatoid Corneal Melt Strategies
| Michéal O Rourke* and Prof Conor Murphy | |
| Royal Victoria Eye and Ear Hospital, Dublin, Ireland | |
| Corresponding author : Michéal O Rourke, Royal Victoria Eye and Ear Hospital, Dublin, Ireland Tel: +353 86 306 1412 E-mail: michaelorourke@rcsi.ie |
|
| Received: March 19, 2015 Accepted: July 16, 2015 Published: July 22, 2015 | |
| Citation: Rourke MO, Murphy C (2015) A Description of the Pathological Features of Rheumatoid Corneal Melt Strategies. J Ophthalmic Pathol 4:3. doi:10.4172/2324-8599.1000161 |
Abstract
A 34 year old woman with a 20 year history of rheumatoid arthritis (RA) presented with a 1 day history of blurred vision in her right eye. Three years earlier she had developed a corneal melt, which had stabilised with a combination of lubricants, topical cyclosporine and a short course of oral prednisolone, and was regularly monitored. Her arthritis had been quiescent for several years on etanercept. Examination of the right cornea revealed a 3 mm descemetocele – an area of corneal stromal melting characterised by total loss of corneal stroma down to Descemet’s membrane, the basement membrane of the corneal endothelium – that was leaking aqueous humour and causing shallowing of the anterior chamber. This is represented in the anterior segment photo (Figure 1) as the dark circular area within the area of corneal scarring. The corneal epithelium was fully intact and the eye was white and quiet. After an attempt at gluing of the perforation, she underwent a tectonic corneal transplant and was prescribed tacrolimus to reduce the risk of allograft rejection. After 3 uneventful years, the corneal transplant was clear, her unaided visual acuity was 20/30 and the tacrolimus was discontinued. On histological examination, the descemetocele was characterised by a fully intact corneal epithelium and Descemet’s membrane with complete loss of corneal stroma (Figure 2). The adjacent stroma was thinned and disorganised and showed a mild inflammatory infiltrate.
Keywords: Rheumatoid Corneal
Discription |
|
| A 34 year old woman with a 20 year history of rheumatoid arthritis (RA) presented with a 1 day history of blurred vision in her right eye. Three years earlier she had developed a corneal melt, which had stabilised with a combination of lubricants, topical cyclosporine and a short course of oral prednisolone, and was regularly monitored. Her arthritis had been quiescent for several years on etanercept. Examination of the right cornea revealed a 3 mm descemetocele – an area of corneal stromal melting characterised by total loss of corneal stroma down to Descemet’s membrane, the basement membrane of the corneal endothelium – that was leaking aqueous humour and causing shallowing of the anterior chamber. This is represented in the anterior segment photo (Figure 1) as the dark circular area within the area of corneal scarring. The corneal epithelium was fully intact and the eye was white and quiet. After an attempt at gluing of the perforation, she underwent a tectonic corneal transplant and was prescribed tacrolimus to reduce the risk of allograft rejection. After 3 uneventful years, the corneal transplant was clear, her unaided visual acuity was 20/30 and the tacrolimus was discontinued. On histological examination, the descemetocele was characterised by a fully intact corneal epithelium and Descemet’s membrane with complete loss of corneal stroma (Figure 2). The adjacent stroma was thinned and disorganised and showed a mild inflammatory infiltrate. | |
| Figure 1: Anterior segment photograph showing a 3mm descemetocele. | |
| Figure 2: Corneal histology of the rheumatoid keratolysis shows complete absence of stroma with only epithelium and Descemet’s membrane remaining. The adjacent stroma is highly disorganised. | |
| Rheumatoid keratolysis is a rare complication of RA which is typically seen in elderly patients with late stage disease [1-4]. Inflammatory symptoms and signs are usually absent, as in this case where silent progressive melting of the stroma led to corneal perforation [4,5]. It has been suggested that matric metaloproteinases, which are activated in the rheumatoid joint are also involved in keratolysis [6] but the pathogenesis of this enigmatic condition is poorly understood. | |
References |
|
|
|
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi