Citiation Analgesia resuscitation current research
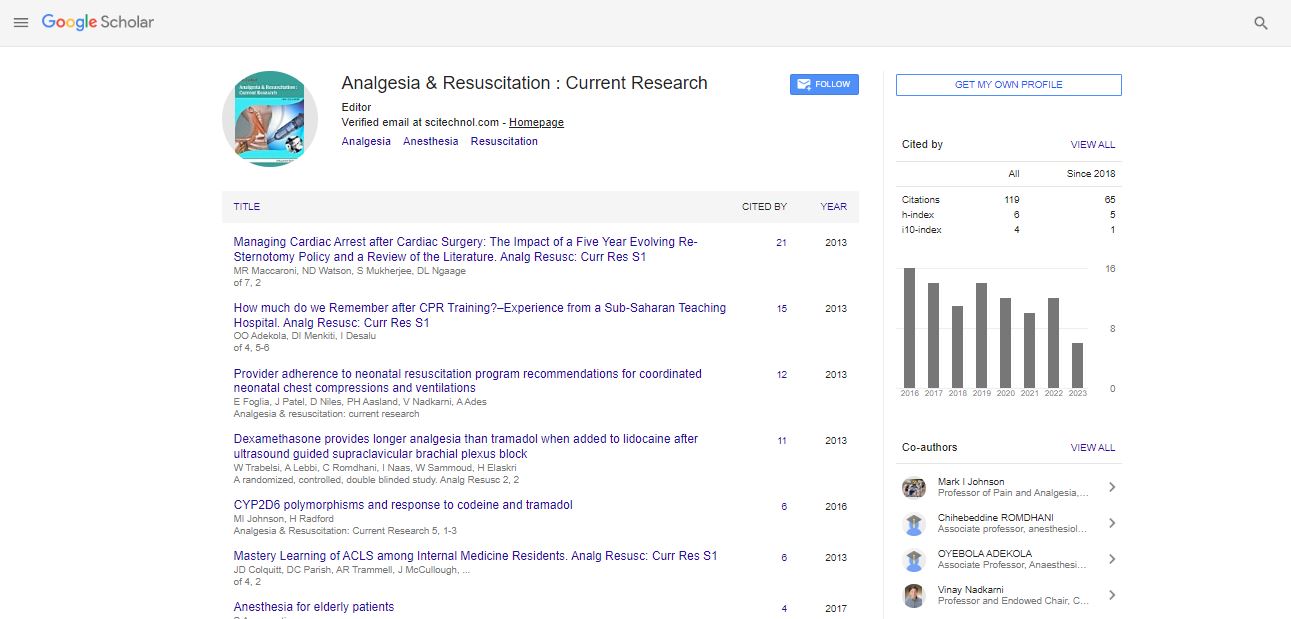
Articles published in Analgesia & Resuscitation : Current Research have been cited by esteemed scholars and scientists all around the world. Analgesia & Resuscitation : Current Research has got h-index 6, which means every article in Analgesia & Resuscitation : Current Research has got 6 average citations.
Following are the list of articles that have cited the articles published in Analgesia & Resuscitation : Current Research.
| 2024 | 2023 | 2022 | 2021 | 2020 | 2019 | 2018 | |
|---|---|---|---|---|---|---|---|
Total published articles |
4 | 37 | 24 | 31 | 12 | 6 | 10 |
Research, Review articles and Editorials |
0 | 0 | 0 | 22 | 0 | 0 | 0 |
Research communications, Review communications, Editorial communications, Case reports and Commentary |
0 | 26 | 15 | 9 | 0 | 0 | 0 |
Conference proceedings |
0 | 0 | 0 | 0 | 0 | 0 | 0 |
Citations received as per Google Scholar, other indexing platforms and portals |
6 | 13 | 12 | 10 | 12 | 14 | 11 |
| Journal total citations count | 119 |
| Journal Impact Factor | 0.40 |
| Journal 5 years Impact Factor | 0.75 |
| Journal CiteScore | 0.65 |
| Journal h-index | 6 |
| Journal h-index since 2017 | 6 |
Phan KM, Lam PV, Kimura BJ (2016 ) “Code Blue” in a 66-Year-Old Man in the Cardiology Department.Chest 150: e37-40. |
Nishiyama T (2016) Effects of nicardipine versus diltiazem on catecholamine secretion and renin-angiotensin-aldosterone system during propofol-fentanyl-nitrous oxide anesthesia. Anaesth Pain & Intensive Care 20: 21-5. |
Eldaba A, Amin SM (2016) A Comparative Evaluation of General Anesthesia versus Spinal Anesthesia Combined with Paravertebral Block for Renal Surgeries: A Randomized Prospective Study. J Anesth Clin Res 7: 2. |
Khajavi MR, Sabouri SM, Moharari RS, Pourfakhr P, Najafi A, et al. (2016) Multimodal analgesia with ketamine or tramadol in combination with intravenous paracetamol after renal surgery. Nephrourol Mon 8: e36491. |
Bandey S, Singh V ( (2016 ) Comparison between IV Paracetamol and Tramadol for Postoperative Analgesia in Patients Undergoing Laparoscopic Cholecystectomy J Clin Diagn Res 10: UC05–UC09. |
Sahib AS, Rashid SA, Jabar HK, Omran MS, Ali MR (2016) Efficacy and Safety Of Acetaminophen Compared To Tramadol After Laparoscopic Cholecystectomy. Inv J Med Sci 4: 3 |
Anand N (2016) Novel Oral Anticoagulant and Efficacy on Atrial Fibrillation Patients. Res Rev J Med Health Sci 5: 3. |
The Enea, Roncon L, MM Gulizia, Azzarito M, Becattini C, et al. (2016) [ANMCO position paper: Use of new oral anticoagulants for the treatment and prevention of pulmonary thromboembolism]. G Ital Cardiol 17: 29S-67S. |
Phan, K. M., Lam, P. V., & Kimura, B. J. (2016). âCode Blueâ in a 66-year-old man in the cardiology department. Chest, 150(2), e37-e40. |
Phan, K. M., Lam, P. V., & Kimura, B. J. (2016). âCode Blueâ in a 66-year-old man in the cardiology department. Chest, 150(2), e37-e40. |
Khajavi, M. R., Sabouri, S. M., Moharari, R. S., Pourfakhr, P., Najafi, A., Etezadi, F., & Imani, F. (2016). Multimodal analgesia with ketamine or tramadol in combination with intravenous paracetamol after renal surgery. Nephro-urology monthly, 8(4). |
Bandey, S., & Singh, V. (2016). Comparison between IV paracetamol and tramadol for postoperative analgesia in patients undergoing laparoscopic cholecystectomy. Journal of clinical and diagnostic research: JCDR, 10(8), UC05. |
Demiroluk, Ã., Abita?ao?lu, S., Göçmen, D. K., Ãzcabi, Y., & Ari, D. E. (2019). Comparison of Analgesic Effects of Paracetamol and Ibuprofen After Laparoscopic Cholecystectomy. Türkiye Klinikleri. Tip Bilimleri Dergisi, 39(3), 278-284. |
SAHIB, A. S., RASHID, S. A., JABAR, H. K., OMRAN, M. S., & ALI, M. R. M. (2016). EFFICACY AND SAFETY OF ACETAMINOPHEN COMPARED TO TRAMADOL AFTER LAPAROSCOPIC CHOLECYSTECTOMY. Innovare Journal of Medical Sciences, 25-27. |
Jahr, J. S., Bergese, S. D., Sheth, K. R., Bernthal, N. M., Ho, H. S., Stoicea, N., & Apfel, C. C. (2018). Current perspective on the use of opioids in perioperative medicine: an evidence-based literature review, national survey of 70,000 physicians, and multidisciplinary clinical appraisal. Pain Medicine, 19(9), 1710-1719. |
Jahr, J. S., Bergese, S. D., Sheth, K. R., Bernthal, N. M., Ho, H. S., Stoicea, N., & Apfel, C. C. (2018). Current perspective on the use of opioids in perioperative medicine: an evidence-based literature review, national survey of 70,000 physicians, and multidisciplinary clinical appraisal. Pain Medicine, 19(9), 1710-1719. |
Jahr, J. S., Bergese, S. D., Sheth, K. R., Bernthal, N. M., Ho, H. S., Stoicea, N., & Apfel, C. C. (2018). Current perspective on the use of opioids in perioperative medicine: an evidence-based literature review, national survey of 70,000 physicians, and multidisciplinary clinical appraisal. Pain Medicine, 19(9), 1710-1719. |
Enea, I., Roncon, L., Gulizia, M. M., Azzarito, M., Becattini, C., Bongarzoni, A., ... & Scherillo, M. (2017). ANMCO Position Paper: the use of non-vitamin K dependent new oral anticoagulant (s) in pulmonary embolism therapy and prevention. European Heart Journal Supplements, 19(suppl_D), D293-D308. |
Enea, I., Roncon, L., Gulizia, M. M., Azzarito, M., Becattini, C., Bongarzoni, A., ... & Scherillo14, M. (2016). Position paper ANMCO: Uso dei nuovi anticoagulanti orali nella terapia e nella prevenzione della tromboembolia polmonare. G Ital Cardiol, 17(9 Suppl 1), 29S-67S. |
Erdem, D., Sözen, ?., Ãak?rca, M., Ãrnek, D., Kany?lmaz, D., Akan, B., & Yast?, A. Ã. (2019). Effect of Nutritional Support Containing Arginine, Glutamine and ?-hydroxy-?-methylbutyrate on the Protein Balance in Patients with Major Burns. Turkish journal of anaesthesiology and reanimation, 47(4), 327. |
Ngaage, L. M., Bai, J., Gebran, S., Elegbede, A., Ihenatu, C., Nam, A. J., ... & Rasko, Y. M. (2019). A 12-year review of patient-reported outcomes after reduction mammoplasty in patients with high body mass index. Medicine, 98(25). |
Brusich, K. T. (2018). Corticosteroids as Adjuvants for Peripheral Nerve Blocks: A Mini Review. Int J Anaesth Res, 1(1), 14-17. |
Hartford, C. T., & Ruano, G. (2018). Fundamental considerations for genetically-guided pain management with opioids based on CYP2D6 and OPRM1 polymorphisms. Pain Physician, 21, E611-E621. |
El-Haj, B. M., Ahmed, S., Garawi, M. A., & Ali, H. S. (2018). Linking aromatic hydroxy metabolic functionalization of drug molecules to structure and pharmacologic activity. Molecules, 23(9), 2119. |
Lyngstad, G., Skjelbred, P., Swanson, D. M., & Skoglund, L. A. (2021). Analgesic effect of oral ibuprofen 400, 600, and 800 mg; paracetamol 500 and 1000 mg; and paracetamol 1000 mg plus 60 mg codeine in acute postoperative pain: a single-dose, randomized, placebo-controlled, and double-blind study. European Journal of Clinical Pharmacology, 1-10. |
Ahmed, S. S., Samad, K., Yousuf, M. S., & Junejo, F. (2020). Paediatric thoracic tumour resection: challenge for an anaesthesiologist. Journal of Ayub Medical College Abbottabad, 32(1), 132-135. |
Wong, C. B., Odamaki, T., & Xiao, J. Z. (2019). Beneficial effects of Bifidobacterium longum subsp. longum BB536 on human health: Modulation of gut microbiome as the principal action. Journal of functional foods, 54, 506-519. |
Friedberg, B. L. (2018). Opioid free anesthesia with BIS/EMG monitored propofol-ketamine. Revista espanola de anestesiologia y reanimacion, 65(5), 243-245. |
Friedberg, B. L. (2020). BIS Monitoring Transformed Opioid-Free Propofol Ketamine Anesthesia From Art to Science for Ambulatory Cosmetic Surgery. Aesthetic Plastic Surgery, 1-4. |
Friedberg, B. L. Ketamine Associated Laryngospasm during Processed EEG Monitored Propofol Sedation Transl Perioper & Pain Med 2020; 7 (4): 291-293. |
Johnson, M. I. (2017). Transcutaneous electrical nerve stimulation (TENS) as an adjunct for pain management in perioperative settings: a critical review. Expert review of neurotherapeutics, 17(10), 1013-1027. |
Crowley, P. D., Stuttgen, V., OâCarroll, E., Ash, S. A., Buggy, D. J., & Gallagher, H. C. (2017). Exposure to 60% oxygen promotes migration and upregulates angiogenesis factor secretion in breast cancer cells. Medical gas research, 7(4), 226. |
Ma, T. M., Paul, B. D., Fu, C., Hu, S., Zhu, H., Blackshaw, S., ... & Snyder, S. H. (2014). Serine racemase regulated by binding to stargazin and PSD-95. Journal of Biological Chemistry, 289(43), 29631-29641. |
Bader, M., Alenina, N., Andrade-Navarro, M. A., & Santos, R. A. (2014). Mas and its related G proteinâcoupled receptors, Mrgprs. Pharmacological reviews, 66(4), 1080-1105. |
Avula, L. R., Buckinx, R., Favoreel, H., Cox, E., Adriaensen, D., Van Nassauw, L., & Timmermans, J. P. (2013). Expression and distribution patterns of Mas-related gene receptor subtypes AâH in the mouse intestine: inflammation-induced changes. Histochemistry and cell biology, 139(5), 639-658. |
Murray, M. J., DeBlock, H., Erstad, B., Gray, A., Jacobi, J., Jordan, C., ... & Mehta, S. (2016). Clinical practice guidelines for sustained neuromuscular blockade in the adult critically ill patient. Critical care medicine, 44(11), 2079-2103. |
Noyes, A. M., & Lundbye, J. B. (2015). Managing the complications of mild therapeutic hypothermia in the cardiac arrest patient. Journal of intensive care medicine, 30(5), 259-269. |
Brown, A. S. Neuromuscular Blocking Agents: Use and Controversy in the Hospital Setting. |
Jenkins, C., Brinkley, K., Alford, H., Costello, K., Korkow, N., Johnson, D., & Fulton, L. V. (2015). Effects of the ResQPOD on kinetics, hemodynamics of vasopressin, and survivability in a porcine cardiac arrest model. Military medicine, 180(9), 1011-1016. |
Jenkins, C., Brinkley, K., Alford, H., Costello, K., Korkow, N., Johnson, D., & Fulton, L. V. (2015). Effects of the ResQPOD on kinetics, hemodynamics of vasopressin, and survivability in a porcine cardiac arrest model. Military medicine, 180(9), 1011-1016. |
Albrecht, E., Kern, C., & Kirkham, K. R. (2015). A systematic review and meta?analysis of perineural dexamethasone for peripheral nerve blocks. Anaesthesia, 70(1), 71-83. |
Kirkham, K. R., Jacot-Guillarmod, A., & Albrecht, E. (2018). Optimal dose of perineural dexamethasone to prolong analgesia after brachial plexus blockade: a systematic review and meta-analysis. Anesthesia & Analgesia, 126(1), 270-279. |
Alarasan, A. K., Agrawal, J., Choudhary, B., Melhotra, A., Uike, S., & Mukherji, A. (2016). Effect of dexamethasone in low volume supraclavicular brachial plexus block: A double-blinded randomized clinical study. Journal of anaesthesiology, clinical pharmacology, 32(2), 234. |
Albrecht, E., Vorobeichik, L., Jacot-Guillarmod, A., Fournier, N., & Abdallah, F. W. (2019). Dexamethasone is superior to dexmedetomidine as a perineural adjunct for supraclavicular brachial plexus block: systematic review and indirect meta-analysis. Anesthesia & Analgesia, 128(3), 543-554. |
Chen, Q., An, R., Zhou, J., & Yang, B. (2018). Clinical analgesic efficacy of dexamethasone as a local anesthetic adjuvant for transversus abdominis plane (TAP) block: a meta-analysis. PloS one, 13(6), e0198923. |
Shin, H. W., Ju, B. J., Jang, Y. K., You, H. S., Kang, H., & Park, J. Y. (2017). Effect of tramadol as an adjuvant to local anesthetics for brachial plexus block: A systematic review and meta-analysis. PloS one, 12(9), e0184649. |
Raj, S. A., Singh, D. R., Charles, S. A. J., & Krishnaveni, N. (2017). Efficacy of tramadol or dexamethasone as an adjuvant to levobupivacaine in ultrasound-guided supraclavicular plexus block for upper limb surgery: A randomized double-blinded controlled study. Anesthesia, essays and researches, 11(3), 567. |
Parveen, S., Jan, M., Taj, A., & Bhat, A. A. (2017). Effect of dexamethasone as an adjuvant with bupivacaine in ultrasound guided single shot supraclavicular brachial plexus block in upper extremity surgeries-a prospective randomized study. International Journal of Research in Medical Sciences, 5(5), 2139-2143. |
Engineer, S. R., Patel, R., Bishnoi, A., & Umrigar, C. M. (2017). Dexamethasone as an adjuvant to bupivacaine in brachial plexus block in upper limb surgery. International Journal of Scientific Reports, 3(10), 265-270. |
Abdel-wahab, A. H., Osman, E. A., & Ahmed, A. Y. (2021). Comparison of postoperative analgesic effects of two doses of dexamethasone in ultrasound-guided transversus abdominis plane block for inguinal hernia repair: a randomized controlled trial. Ain-Shams Journal of Anesthesiology, 13(1), 1-8. |
Bedocs, P., Capacchione, J., Potts, L., Chugani, R., Weiszhar, Z., Szebeni, J., & Buckenmaier, C. C. (2014). Hypersensitivity reactions to intravenous lipid emulsion in swine: relevance for lipid resuscitation studies. Anesthesia & Analgesia, 119(5), 1094-1101. |
Fulton, L. V., Fabich Jr, R. A., Bhatta, J., Fletcher, B., Leininger, K., Lienesch, K., ... & O'Sullivan, J. (2016). Comparison of resuscitative protocols for bupropion overdose using lipid emulsion in a swine model. Military medicine, 181(5), 482-487. |
Fulton, L. V., Fabich Jr, R. A., Bhatta, J., Fletcher, B., Leininger, K., Lienesch, K., ... & O'Sullivan, J. (2016). Comparison of resuscitative protocols for bupropion overdose using lipid emulsion in a swine model. Military medicine, 181(5), 482-487. |
McRae, M. E., Chan, A., Hulett, R., Lee, A. J., & Coleman, B. (2017). The effectiveness of and satisfaction with high-fidelity simulation to teach cardiac surgical resuscitation skills to nurses. Intensive and Critical Care Nursing, 40, 64-69. |
Dunning, J., Levine, A., Ley, J., Strang, T., Lizotte Jr, D. E., Lamarche, Y., ... & Bakaeen, F. G. (2017). The society of thoracic surgeons expert consensus for the resuscitation of patients who arrest after cardiac surgery. The Annals of Thoracic Surgery, 103(3), 1005-1020. |
McRae, M. E., Chan, A., Lee, A. J., Hulett, R., & Coleman, B. (2017). Team-based learning improves staff nursesâ knowledge of open-and closed-chest cardiac surgical resuscitation. Dimensions of Critical Care Nursing, 36(1), 60-67. |
Michaelis, P., & Leone, R. J. (2019). Cardiac arrest after cardiac surgery: an evidence-based resuscitation protocol. Critical care nurse, 39(1), 15-25. |
Stueben, F. (2017). Implementation of a simulation-based cardiac surgery advanced life support course. Clinical Simulation in Nursing, 13(9), 432-435. |
Ley, S. J. (2015, June). How should we manage arrest following cardiac surgery?. In Seminars in cardiothoracic and vascular anesthesia (Vol. 19, No. 2, pp. 87-94). Sage CA: Los Angeles, CA: SAGE Publications. |
Ley, S. J. (2019). Cardiac surgical resuscitation: State of the science. Critical Care Nursing Clinics, 31(3), 437-452. |
Mendoza, J. L. A., Estrada, V. H. N., Pérez, J. C. D., Senior, J. M., Leiva, E. H., Valencia, A. A., ... & Delgado, J. F. (2020). Consenso colombiano de cuidados perioperatorios en cirugÃa cardiaca del paciente adulto. Acta Colombiana de Cuidado Intensivo, 20(2), 118-157. |
Marler, G. S., Molloy, M. A., Engel, J. R., Walters, G., Smitherman, M. B., & Sabol, V. K. (2020). Implementing Cardiac Surgical UnitâAdvanced Life Support Through Simulation-Based Learning: A Quality Improvement Project. Dimensions of Critical Care Nursing, 39(4), 180-193. |
Roberts, M., & Miller, S. A. (2019). Implementation of an Innovative Nurse-Driven Resuscitation Protocol. JONA: The Journal of Nursing Administration, 49(7/8), 372-376. |
Yan, W., Moran, H. R. M., Zelentsov, I., Eikelboom, R., Lodewyks, C., Strumpher, J., & Arora, R. C. (2021). Improving outcomes after low-risk coronary artery bypass grafting: understanding phase of care mortality analysis, failure to rescue and recent perioperative recommendations. Current Opinion in Cardiology, 36(5), 644-651. |
Dunning, J., Levine, P. A., Ley, F. J., Strang, T., Lizotte, M. D., MPAS, F. Y. L., ... & Haft, J. STS expert consensus for the resuscitation of patients who arrest after cardiac surgery. |
Dunning, J., Levine, P. A., Ley, F. J., Strang, T., Lizotte, M. D., MPAS, F. Y. L., ... & Haft, J. STS expert consensus for the resuscitation of patients who arrest after cardiac surgery. |
Leiva, EH, Valencia, AA, Serna, JFE, Castell, CD, Ramos, RC, Beltrán, N., ... & Delgado, JF (2020). Intensive Care. |
Barsuk, J. H., Cohen, E. R., Wayne, D. B., Siddall, V. J., & McGaghie, W. C. (2016). Developing a simulation-based mastery learning curriculum: lessons from 11 years of advanced cardiac life support. Simulation in Healthcare, 11(1), 52-59. |
Dorri, S., & Hakimi, H. (2017). The effect of mastery learning model for suction and oxygen therapy skills in nursing students. Research in Medical Education, 9(4), 19-10. |
Dorri, S., & Shamsi, A. (2018). The Role of Mastery Learning in Clinical Education: A Systematic Review. Strides in Development of Medical Education, 15(1). |
Dorri, S., & Shamsi, A. (2018). The Role of Mastery Learning in Clinical Education: A Systematic Review. Strides in Development of Medical Education, 15(1). |
Brown, S. (2015). Critical Synthesis Package: Advanced Cardiac Life Support (ACLS) Checklists for Simulation-Based Education. MedEdPORTAL, 11. |
Everett-Thomas, R., Turnbull-Horton, V., Valdes, B., Valdes, G. R., Rosen, L. F., & Birnbach, D. J. (2016). The influence of high fidelity simulation on first responders retention of CPR knowledge. Applied Nursing Research, 30, 94-97. |
Everett-Thomas, R. (2017). Cardiopulmonary resuscitation knowledge among nursing students: a questionnaire-based study. Anadulu Kardiyoloji Dergisi: AKD, 17(2), 146. |
Ghirmai, F. A., Weldeghiorgis, G. G., Bahlebi, T. T., & Tesfamariam, E. H. (2020). Effectiveness Of Structured Training Programme Regarding Adult Basic Life Support On Knowledge Of NursesIn Zoba Maekel And National Referral Hospitals, Eritrea, 2018. |
Rikhotso, M., Perrie, H., Scribante, J., & Jooma, Z. (2021). Cardiopulmonary resuscitation skills profile and knowledge of nurses working in an academic hospital. SA Heart, 18(1), 40-46. |
Solevåg, A. L., Cheung, P. Y., O'Reilly, M., & Schmölzer, G. M. (2016). A review of approaches to optimise chest compressions in the resuscitation of asphyxiated newborns. Archives of Disease in Childhood-Fetal and Neonatal Edition, 101(3), F272-F276. |
Solevåg, A. L., & Schmölzer, G. M. (2017). Optimal chest compression rate and compression to ventilation ratio in delivery room resuscitation: evidence from newborn piglets and neonatal manikins. Frontiers in pediatrics, 5, 3. |
Te Pas, A. B., Sobotka, K., & Hooper, S. B. (2016). Novel approaches to neonatal resuscitation and the impact on birth asphyxia. Clinics in perinatology, 43(3), 455-467. |
Patel, S., Cheung, P. Y., Lee, T. F., Pasquin, M. P., Lu, M., OâReilly, M., & Schmölzer, G. M. (2020). Asynchronous ventilation at 120 compared with 90 or 100 compressions per minute improves haemodynamic recovery in asphyxiated newborn piglets. Archives of Disease in Childhood-Fetal and Neonatal Edition, 105(4), 357-363. |
Solevåg, A. L., Cheung, P. Y., & Schmölzer, G. M. (2014). Chest compressions and ventilation in delivery room resuscitation. NeoReviews, 15(9), e396-e402. |
Myers, P., & Gupta, A. G. (2020). Impact of the revised NRP meconium aspiration guidelines on term infant outcomes. Hospital pediatrics, 10(3), 295-299. |
Schmölzer, G. M. (2016). Remember fatigue during neonatal cardiopulmonary resuscitation and don't forget to change resuscitators. Acta Paediatrica (Oslo, Norway: 1992), 105(8), 866-867. |
Sloane, A. J., Kenaley, K. M., & Favara, M. T. (2021). Assessment of temporal variations in adherence to NRP using video recording in the delivery room. Resuscitation plus, 8, 100162. |
Patel, S. (2020). Hemodynamic Differences in Recovery Following Chest Compression with Asynchronous Ventilation Using Chest Compression Rates of 90/min, 100/min, or 120/min in a Porcine Model of Neonatal Asphyxia. |
Patel, S. (2020). Hemodynamic Differences in Recovery Following Chest Compression with Asynchronous Ventilation Using Chest Compression Rates of 90/min, 100/min, or 120/min in a Porcine Model of Neonatal Asphyxia. |
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi