Research Article, J Clin Exp Oncol Vol: 5 Issue: 3
Olive Leaf Extract Reduces Myeloid-Derived Suppressor Cells, and Modulates the Function of Residual Cells in Experimental Model of Melanoma
| Mahboubeh Ashourpour1, Afshin Namdar2, Nasim Kheshtchin3, Morteza Hafezi1, Najmeh Khosravianfar1, Maryam Ajami4, Bahram Delfan5,Yaser Azizi6,7, Samaneh Arab8, Reza Mirzaei3, Abbas Mirshafiey1, Jamshid Hadjati3, Alireza Razavi1* | |
| 1Department of Pathobiology, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran | |
| 2Department of Immunology, School of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran | |
| 3Department of Immunology, School of Medicine, Tehran University of Medical Sciences, Tehran, Iran | |
| 4Department of Immunology, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran | |
| 5Department of Pharmacology, School of Medicine, Lorestan University of Medical Sciences, Khorram Abad, Iran | |
| 6Department of Physiology, Faculty of Medicine, Iran University of Medical Sciences, Tehran, Iran | |
| 7Physiology Research Center, Department of Physiology, School of Medicine, Iran University of Medical Sciences, Tehran, Iran | |
| 8Department of Molecular Medicine, School of Advanced Technology, Tehran University of Medical Sciences, Tehran, Iran | |
| Corresponding author : Dr. Alireza Razavi Department of Pathobiology, School of Public Health, Tehran University of Medical Sciences Tehran, Iran Tel: +98 21 8897 0821 Fax: +98 21 8897 0824 E-mail: razavial@tums.ac.ir |
|
| Received: May 04, 2016 Accepted: June 23, 2016 Published: June 27, 2016 | |
| Citation: Ashourpour M, Namdar A, Kheshtchin N, Hafezi M, Khosravianfar N (2016) Olive Leaf Extract Reduces Myeloid-Derived Suppressor Cells, and Modulates the Function of Residual Cells in Experimental Model of Melanoma. J Clin Exp Oncol 5:3. doi:10.4172/2324-9110.1000159 |
Abstract
Background: Immunosuppression in melanoma is mediated by increased accumulation of Myeloid Derived Suppressor Cells (MDSCs). Olive Leaf Extract (OLE) has been developed as a natural anti-inflammatory, anti-oxidant, anti-proliferative and antiapoptotic agent on cancer immunotherapy.
Objective: To investigate whether OLE could inhibit MDSCs, enhance anti-tumor activities and consequently increase the survival rate of the murine melanoma model.
Methods: The C57BL/6 mice were inoculated subcutaneously with B16/F10 melanoma tumor cell lines. Induced mice were orally treated with 500 mgkg-1 of olive extract per kg of body weight for 8 consecutive days. The frequency and function of MDSCs and induction of inflammatory mediators as well as tumor growth and survival rate were assessed in treated and untreated mice.
Results: The results of current study revealed that the optimal dose of OLE (500 mgkg-1) reduced the tumor growth (40%), and prolonged mice survival (25%) by significant decreasing (P<0.05) the number (over 50%), and suppressive function of MDSCs (over 60%) (P<0.05). OLE was also significantly (P<0.05) down regulated the induction of inflammatory agents in melanoma-bearing mice (over 50%) at the applied dose (500 mgkg-1).
Conclusion: Therefore, these results altogether provided some evidence that regulation of immunosuppression were the possible therapeutic effects of OLE in tumor cells.
Keywords: Melanoma; Myeloid-derived suppressor cells; Olive leaf extract
Keywords |
|
| Melanoma; Myeloid-derived suppressor cells; Olive leaf extract | |
Introduction |
|
| Malignant melanoma is the most growing, metastatic and high risk type of skin cancers that its annual incidence has been increased dramatically over the few past decades, particularly in the younger generation [1]. Despite the numerous researches in cancer, results have indicated the low responses of malignant melanoma cancer to various conventional therapies such as radiation and chemotherapy. Although these conventional therapies have been effective in the treatment of some types of tumors, they are very toxic and nonspecific [1,2]. Beside, several studies have shown that low responses to immunotherapies in melanoma highly depend on a wide range of immunosuppression mechanisms in tumor microenvironment [3]. Among these mechanisms, myeloid derived suppressor cells (MDSCs) play vital roles in progression and metastasis of melanoma by exhibiting the immunosuppressive effects [4,5]. Myeloid derived suppressor cells as a heterogeneous population of immature myeloid cells have accumulated in the blood, tumors, lymph nodes, and spleens of human and experimental animal models, especially in mice [6-8]. Phenotypically, mouse MDSC are characterized as Gr1+ CD11b+ cells [9], which regulates T cell proliferation and activation through various pathways, such as Arginine depletion, Reactive Oxygen Species (ROS) production [10,11] and inducible Nitric Oxide Synthase (iNOS) [12-14]. Furthermore, MDSCs expansion as an immune suppression mechanism develops tumor progression in chronic inflammation [15-17]. Increasing of MDSCs could inhibit the responses of antigen specific T cell. Suppressive factors, such as inducible nitric oxide synthase (iNOS) and reactive oxygen species (ROS) [7,8] will mediate this inhibition. Thus, a number of researchers are targeting the elimination of MDSCs by different therapeutic strategies to overcome immune suppression in tumors [18]. Chronic inflammation develops tumor progression via inducing immunosuppression mechanisms, such as MDSCs expansion [15-17]. Many synthetic and herbal compounds have been included in therapeutic strategies due to their anti-inflammatory effects in chronic inflammatory diseases related to the immune system [19,20]. Herbal products, the natural, without significant side effects, have contributed to cancer therapy [21]. Among the herbs, Olive leaf extract (OLE) has provided lots of definite clinical evidences for its disease preventing characteristics [22]. The OLE with its main bioactive constituents was shown to have antioxidant, anti-inflammatory, hypoglycemic, anti-microbial, antihypertensive, neuroprotective, anti-viral, and anti-cancer capacities [23-27]. And also, anti-proliferative and anti-apoptotic effects of OLE have been recently reported to inhibit various tumor cell lines in vitro [28,29]. These bioactive constituents with proven evidences for health benefits are Oleuropein, Hydroxytyrosol, and also polyphenolic plant metabolites, such as Apigenin-7-glucoside, Verbascoside, and Luteolin-7-glucoside [30,31]. In vitro, oleuropein and its closely related metabolite, hydroxytyrosol, performed a wide range of pharmacological effects and anti-inflammatory enhancements [32] through scavenging of free radicals and also inhibition of 5-lipoxygenase and 12-lipoxygenase activities [33]. Moreover, the OLE inhibited the ulcerative colitis disease in rats through a significant reducing of the increasing levels of TNF-α and interlukin-2 markers [34]. Furthermore, OLE inhibited carcinogenesis, and prevented increases in the VEGF and COX-2 level expression in mice skin tumors [27]. In other hands, it has been represented that blockig inflammation mediators may facilitate immune surveillance and antitumor immunity through reducing accumulation of MDSCs [35-37]. With this background, we sought to elucidate whether OLE with anti-inflammatory capacity could modulate the content of MDSCs in animal melanoma model in order to augment anti-cancer immune responses. Although previous information has shown the anti-cancer properties of OLE on various cell lines in vitro, little attention has been paid to its effects on the immune system and immune regulatory cells including MDSCs. Therefore, in the current research, we investigated the potential anti-inflammatory effects of OLE in experimental model of melanoma. We further examined the possible effect of OLE mediated anti-inflammatory mechanisms on MDSCs accumulation and function. The results of this study demonstrated new insights for the anti-cancer properties of OLE as an immunotherapeutic compound in inflammation-associated cancers. | |
Materials and Methods |
|
| Preparation of OLE and quantification of the components by HPLC | |
| The dried olive leaf extract was prepared through an ethanolic extraction process in the Herbal Medicine Institute (Lorestan, Iran). The extract patently filtered by EFLA® HyperPure procedures, and then the crude filtrated part of the extract was air dried. The major types of phenolic constituents of crude extract were measured through chromatographic analysis using high-performance liquid chromatography (HPLC) in 1 g of dry crude extract at 240 nm wavelength [38]. The main phenolic compositions of OLE were oleuropein (356 mg/g), tyrosol (3.73 mg/g), hydroxytyrosol (4.89 mg/g) and caffeic acid (49.41 mg/g) of the dry extract [39]. | |
| Mice, cell line and tumor model | |
| Six- to eight- week old (mature) female C57BL/6 mice were purchased from Pasteur Institute of Iran. Animal care was performed in accordance with the guideline of Tehran University of Medical Sciences throughout the experiment. The mouse melanoma cell line, B16/F10, was obtained from Pasteur Institute of Iran and the Mycoplasma contamination of cell culture was tested. The C57BL/6 mice were inoculated subcutaneously in the right flank with 5×105 melanoma tumor cells of B16/F10. Tumor surfaces (mm2) were determined using the formula (long axis × short axis) every 2 days based on caliper measurements. | |
| Tumor establishment and OLE administration | |
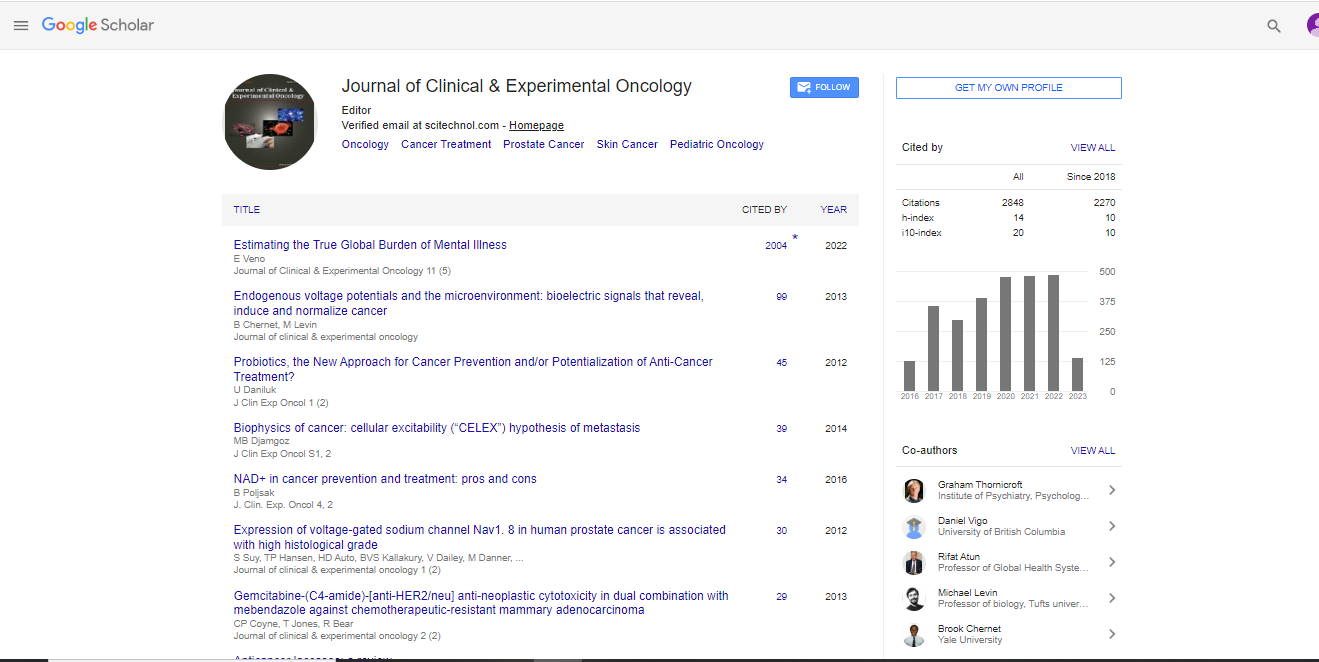
| Mice with detected tumors were randomly divided into two groups of eight mice (control and treatment groups). Mice in treatment group were orally received 500 mg olive extract per kg of body weight for 8 consecutive days that started immediately after tumors detection. The optimal dose of the extract was chosen based on previous studies [27,34,40] as well as our pilot study (data are shown in Figure 1). The mice in control group also were treated orally with the same volume of distilled water. All treatments were applied at the same time and volume. The mice in control and treatment groups were sacrificed 24 hours after the last gavage by cervical dislocation. | |
| Figure 1: OLE treatment decreases the percentage of Gr1+ CD11b+ cells in F10 tumor bearing mice. C57BL6 mice were inoculated with 5×105 B16/F10 cell line. Mice in treatment groups were orally received 250 and 500 mg olive extract per kg of body weight for 8 consecutive days that started immediately after tumors detection. The mice in control group also received the same volume of distilled water by gavage. Mice splenocytes were harvested one day after the last OLE treatment (day 14), and then labeled with anti- Gr-1 and anti- CD11b antibodies. A) ├»┬Č┬?ow cytometry plots show percent of Gr-1+ CD11b+ cells in mice treated with two different OLE doses versus untreated mice. B) Bar Graph Represents the mean percentage of Gr-1+ CD11b+ cells in mice receiving different doses of OLE in comparison to untreated mice. n=4; * significant at P<0.05. (Bars indicate mean ± SD). | |
| Flow cytometry | |
| 105 splenocytes were resuspended in phosphate buffered saline (PBS) with fetal calf serum (FCS) 1% and incubated with fluorescently labeled monoclonal antibodies accompanied by related fluorochrome labeled isotype control monoclonal antibodies for 30 minutes at 4°C. Samples were then washed with PBS. Fluorescence data were analyzed by FACS Diva software (BD Biosciences, San Jose, CA) and FlowJo software (TreeStar, Ashland, OR). | |
| Isolation of splenic MDSCs | |
| Splenocytes from both treatment and control groups of C57BL/6 mice were harvested and dissociated mechanically under sterile situation, and red blood cells were lysed using 4% ammonium chloride lysis buffer. Splenic Gr1+ CD11b+ cells were purified via anti- Gr-1 antibody and streptavidin-magnetic beads according to the manufacturer’s instructions (Miltenyi Biotech, Germany). The purity of Gr1+ CD11b+ cell population was figured by flow cytometry and exceeded 90% through this procedure. | |
| ROS detection | |
| Splenocytes from both OLE-treated and untreated mice were incubated with 2 μmol/L dichlorodihydrofluorescein diacetate (DCFDA) dye (Sigma-Aldrich, USA), at 37°C for 30 minutes in the dark. Afterwards, samples were labeled with allophycocyanin (APC)- conjugated anti-Gr1 and phycoerythrin (PE)-conjugated anti-CD11b antibodies. Cells were then washed with PBS following incubation on ice for 20 min. Then, the level of ROS was detected by flow cytometry. | |
| Nitric Oxide (NO) detection | |
| Nitric oxide production was determined using Greiss reagent (0.1% N-1- naphthylethylenediamine dihydrochloride and 1% sulfanilamide in 5% HCL). Briefly, 105/200 μl of treated and untreated splenocytes were cultured in complete medium in 96 –well round bottom plates in the presence of lipopolysacharide (LPS, Sigma) with final concentration of 1 μg/ml and were incubated at 37°C for 24 hours. Then 50 μl Sulfanilamide 1% was added to the culture supernatants, and incubated for 5 minutes at room temperature in the dark. Next, 50 μl of naphthylethylenediamine dihydrochloride 0.1% was added to the wells. After 15 minutes, the absorbance value of the mixture was measured at 550 nm using ELISA Reader. Nitrite concentrations were determined by comparing the absorbance value of the test samples to a standard curve of serial dilution of 0.25 mM sodium nitrite. | |
| Real-Time PCR | |
| RNA was extracted with Trizol-Reagent (Qiagen). 1μg of RNA was reverse transcribed into complementary DNA (cDNA) using QuantiTect Reverse Transcription kit (Qiagen). cDNAs were quantified by real-time PCR using a SYBR Green Real-time PCR mastermix (Primer design, UK) on an ABI 7500 detection system (Applied biosystems). Relative mRNA levels were determined using the comparative CT method (ΔCT). Values were expressed relative to endogenous β-actin. The following PCR primers were used: β-actin forward, 5’-GGTCATCACTATTGGCAACG-3’; β-actin reveres, 5’ACGGATGTCAACGTCACACT-3’; VEGF forward, 5’-GCGGAGAAAGCATTTGTTTG- 3’; VEGF reveres, 5’-TCTTTCCGGTGAGAGGTCTG- 3’; TGF-β forward, 5’-ACCATGCCAACTTCTGTCTG- 3’; TGF-β reverse, 5’- CGGGTTGTGTTGGTTGTAGA -3’; COX-2 forward, 5’-CTGACCCCCAAGGCTCAAAT-3’; COX-2 reverse, 5’-ACCTCTCCACCAATGACCTGA-3’; TNF-α forward, 5’-TGAGCACAGAAATGATC-3’; TNF-α reveres 5’-GGACTTCT CAT CCCTTTGG-3’; iNOS forward, 5’-AGTGGTGTTCTTTGCTTC -3’; iNOS reverse, 5’-GCTTGCCTTATACTGGTC-3’; arginase forward, 5’- AAGAAAAGGCCGATTCACCT-3’; arginase reveres 5’-CACCTCCTCTGCTGTCTTCC-3’. | |
| Statistical analysis | |
| Parametric and nonparametric means comparisons were performed through a Student’s t-test or Mann-Whitney test. Survival curves were analyzed by Log-rank test. All tests were performed with Graph Pad Prism software (version 5.0) at the 5% probability level. | |
Results |
|
| Effect of OLE on the number of splenic MDSCs in Melanoma- bearing mice | |
| The modulatory effect of two different doses of OLE (250 and 500 mg kg-1) on splenic MDSC content was assessed in tumor-challenged mice. In this procedure, cell surface markers Gr-1 and CD11b were monitored for the MDSCs counts. The results were presented in Figure 1A and B. According to our results, 500 mgkg-1 of OLE could significantly decrease MDSC quantity in melanoma bearing mice spleens (P<0.05). Whereas, at lower dose of OLE (250 mgkg-1) no significant change in MDSCs count was observed. The average number of MDSCs was reduced about 10% and 56% at 250 and 500 mgkg-1 respectively versus control group (Figure 1A and B). | |
| Effect of OLE on MDSCs suppressive function | |
| We next explored whether the optimal dose of OLE (500 mgkg-1) may reduce the suppressive function of residual MDSCs. The mean fluorescence intensity (MFI) analysis of DCFDA after staining of spleen cells with anti-Gr-1, anti-CD11b antibodies and gating on the Gr1+ CD11b+ population indicated that the levels of ROS production were decreased by the population of Gr1+ CD11b+ cells in the treated group. OLE treatment (500 mgkg-1) inhibited ROS production (P<0.01) with significant difference compared to untreated group (Figure 2A, B and C). Consistent with the ROS results, the level of NO production significantly decreased (P<0.05) following OLE treatment (Figure 2D). These data demonstrated that 500 mgkg-1 of OLE applied dose preferentially reduced the NO production about 75% compared to untreated mice. Similar with NO and ROS, the expression of iNOS and arginase-1 have been involved in MDSCs suppressive function. In current study, the level of iNOS and Arginase expression in splenic MDSCs was analyzed. For this purpose, RNA from sorted splenic MDSCs was assessed using RT-PCR for iNOS and ARG expression. The results obtained from tumor-challenged mice indicated that the expression of iNOS and arginase mRNA expression (Figure 2D and E) with almost similar patterns were drastically and significantly decreased in MDSCs isolated from mice (P<0.05). The inhibitory effect of OLE on iNOS and arginase mRNA expression was seen in 500 mgkg-1 of OLE applied dose about 64% and 83% over control group, respectively. | |
| Figure 2: The Effects of OLE treatment on MDSCs function. A) Flow cytometry analysis of gated CD11b+ Gr-1+ cells positive for DCFDA in OLE-treated and untreated tumor-challenged mice. Mice spleen cells were incubated with DCFDA. Mean fluorescence intensity shows the ROS level in MDSCs from the indicated groups. B) Mean fluorescent intensity (MFI) representing ROS level in MDSCs from the treated and untreated mice. C) Percent of MDSCs positive for DCFDA. D) Concentration of NO in tumor-challenged mice splenocytes in the absence and presence of OLE using Griess reagent. Data are the mean ± SD of triplicate wells. E) The effect of OLE on mRNA expression levels of iNOS and arginase in splenic MDSCs from treated and untreated mice. Gr-1+ cells were sorted from mice spleens. RNA was then extracted from the sorted cells, and expression levels of iNOS and Arginase were measured by quantitative real-time PCR. A representative out of three independent experiments is depicted (n=4; * significant at P<0.05). | |
| Effect of OLE on the expression of inflammatory genes in tumor | |
| Importantly, several mechanisms have been implicated in suppressive functions of MSDCs through anti-tumoral response of the immune system in vivo. To optimally activate the anti-tumor immunity, immunomodulatory treatments must inhibit inflammatory effects through downregulation of some mediators responsible for MDSCs development, such as TNF-α, COX-2, TGF-β and VEGF. Therefore, we finally investigated the effect of OLE on indicated inflammatory genes (Figure 3A and B) in the tumors (left graph) and splenic cells (right graph) of treated and untreated mice. Altogether, these results showed that OLE administration reduced expression in all factors. In case of TNF-α mRNA, the gene expression analysis showed a significant reduction in the OLE treatment group (500 mgkg-1) in both tumors (P<0.05) and spleens (P<0.05) of treated mice with the same trend over control (Figure 3A and B). The results of Cox-2 mRNA response to OLE exposure emphasized the possibility of the OLE effect on gene downregulation in both microenvironments. Administration of OLE effective dose (500 mgkg-1) led to a significant decrease in COX-2 mRNA level in spleens (60%) and tumors (86%) compared to control group (P<0.05) (Figure 3A and B). Also, based on our results, OLE optimal dose numerically, but non-significantly decreased the mRNA expression of both TGF-β and VEGF (Figure 3A and B). | |
| Figure 3: Effect of OLE administration on the expression of inflammatory genes. A) Gene expression measured at the mRNA level for TNF-α, COX-2, TGF-β and VEGF in tumor mass of treated and untreated melanoma-bearing mice. B) Gene expression measured at the mRNA level for TNF-α, COX-2, TGF-β and VEGF in spleen of treated tumor-challenged mice versus untreated mice. Total RNA was extracted from tumors and spleens of individual mice and subjected to RT-PCR following cDNA synthesis. A representative out of three independent experiments is depicted (n=4; * significant at P<0.05). | |
| Effect of OLE on tumor growth and survival in B16/F10 Tumor- bearing mice | |
| We finally evaluated melanoma tumor growth and survival in tumor-challenged mice treated with OLE applied dose (500 mgkg-1) and compared it to untreated mice. The current study represented that a significant reduction of tumor size was seen in OLE-treated mice compared to untreated mice (P<0.01) (Figure 4A, B and C). Tumor sizes were around 400 mm2 at the end of the experiment. Moreover, as shown in Figure 4D, the increased survival rate of treated mice (numerically, but non-significantly) was obtained at the OLE effective dose (about 25%) in comparison to control group. | |
| Figure 4: Effect of OLE treatment on tumor growth rate and survival in tumor-bearing mice. C57BL/6 mice were injected subcutaneously with 5×105 B16-F10 melanoma cells. Mice tumor size was measured using caliper every two days. Afterwards, treatment with OLE (500 mgkg-1) was performed 7days after tumor injection. A and B) Graphs show the mean tumor growth/day in mice different groups. C) Tumor growth curves in treated mice compared to untreated mice. D) Survival of the animals in each group was monitored and the respective curves are given (n=8; * significant at P<0.05). | |
Discussion |
|
| The malignant tumors are commonly grown and developed in the immunosuppressive micro-environment. The expansion of MDSCs as major suppressive cells has been seriously promoted the tumor occurrence in a lot of animal tumor models with different types of cancers. Despite a number of strategies have been explored to either mediate or eliminate the immunosuppressive functions of MDSCs, the preclinical mouse models and clinical studies still represent a major obstacle for effective tumor immunotherapy [3,7,8,41]. Over the past decade, research findings have documented proven evidences that herbal compared to chemical drugs not only may have anti-cancer and anti-inflammatory properties that inhibit tumor development, but also have several advantages such as reduction of side effects and less likely to cause dependency [21]. Since it is well-established that chronic inflammation leads to the accumulation of MDSCs [15-16,35-37], and regarding the anti-inflammatory properties of OLE [26,27], we hypothesized that OLE by blocking or inhibiting MDSCs can be evaluated as a new therapeutic compound. The results of current study indicated that the effective dose of OLE (500 mgkg-1) was contributed to a significant reduction in MDSCs that indicated the anti-tumor effect of OLE in limiting MDSCs accumulation. It is well established that immune suppression of MDSCs is mediated by ROS and NO as well as arginase and iNOS levels, which is associated with inhibition of anti-tumor T cell responses [42,43]. In fact, ROS and arginase mediate MDSCs suppressive functions via increasing NADPH oxidase activity [42,43], and arginine catabolism, respectively [44]. Therefore, we explored whether OLE could attenuates ROS and NO production and also arginase and iNOS levels in MDSCs population. We found that OLE drastically reduced production of ROS, which could be related to the reduced number of MDSCs. This result was more interesting when we observed that OLE down regulated the mRNA expression level of arginase and iNOS. Therefore, OLE modulated the suppressive activity of residual MDSCs isolated from melanoma-bearing mice. More researches are needed to identify the mechanism of the observed effect of OLE on MDSCs in the spleen. Since treatment of tumorbearing mice with OLE was led to reduction of MDSCs number and functions, we investigated whether this depletion might contribute to reduction of tumor growth and also prolongation of mice survival. By monitoring the tumor dimensions following tumor inoculation during the time of 8 days, 500 mgkg-1 of OLE was contributed to a reduction in tumor growth, and prolongation of mice survival compared to the untreated group. This finding was in consistent with the result of Mijatovic et al, which indicated the anti-tumor potential of OLE in B16 tumor model [29]. As it seems, the effect of OLE on down-regulating the myeloid suppressor population, is related to the rate of the tumor growth. It looks that the suppressor cells, which are in the focus of this study are relevant for obtaining results, concerning the outcome of disease. As inflammation has a substantial role in the induction and accumulation of MDSCs and tumor progression [15-17], we measured the expression of some inflammatory mediators such as TNF-α, COX-2, VEGF and TGF-β in spleens and tumors of OLE treated mice. Our results showed that OLE downregulated the levels of indicated genes in both tumors and spleens. This result provided a mechanism for the MDSCs reduction, which led to decrement in tumor-associated immunosuppression. It seems that reduction of inflammatory mediators by OLE has played an important role in reducing MDSCs. However, these findings did not exclude the effect of OLE on other inflammatory agents such as STAT-3 that was involved in MDSCs expansion [45]. Also the possible importance of epigenetic mechanisms in the gene expression regulation should be mentioned. Besides, more research is needed to identify other inflammatory agents involved in MDSCs accumulation. The findings of Wang [46] and Gong et al. [26] have provided consistent support to our results in anti-inflammatory activity of OLE. Further researches are needed to identify the active biological agents responsible for the observed benefit. Since the use of total extracts requires high doses, it would be difficult to use the extract in medicinal form. But in case of active components of OLE, such as oleuropein and hydroxyl tyrosol, the use of lower doses is possible. Our investigation clarified the brilliant impacts of OLE on the immune system and immuneregulation of MDSCs in mice through NO and ROS reduction as well as inflammatory agents associated with induced MDSCs accumulation. Depletion of MDSCs led to reduced tumor growth and increased survival in melanoma bearing mice treated with the optimal dose of OLE. Importantly, OLE was well tolerated in mice, and no adverse effect was seen following administration. Thus, this result might open a new window on developing more effective melanoma therapeutic strategies due to its repressing action on immunosuppression mechanisms. | |
Acknowledgments |
|
| This study was supported by Tehran University of Medical Sciences (grant 23146) and the Iran National Science Foundation (INSF) (grant 92002005). | |
References |
|
|
|
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi