Research Article, J Pharm Drug Deliv Res Vol: 4 Issue: 2
In Vitro Characterization of the Percutaneous Absorption of Lorazepam into Human Cadaver Torso Skin, Using the Franz Skin Finite Dose Models
| August S Bassani, Daniel Banov and Ha Phan* |
| Professional Compounding Centers of America (PCCA), USA |
| Corresponding author : Ha Phan 9901 South Wilcrest Dr, Houston, TX 77099, USA Tel: 800-331-2498 Ext. 1127; Fax: 800-874-5760 E-mail: HPhan@pccarx.com |
| Received: August 11, 2015 Accepted: September 03, 2015 Published: September 06, 2015 |
| Citation: Bassani AS, Banov D, Phan H (2015) In Vitro Characterization of the Percutaneous Absorption of Lorazepam into Human Cadaver Torso Skin, Using the Franz Skin Finite Dose Model. J Pharm Drug Deliv Res 4:2. doi:10.4172/2325-9604.1000131 |
Abstract
In Vitro Characterization of the Percutaneous Absorption of Lorazepam into Human Cadaver Torso Skin, Using the Franz Skin Finite Dose Models
Objective
Lorazepam is a sedative that may be used for the management of anxiety, insomnia, and chemotherapy-induced nausea and vomiting. Lorazepam can be incorporated into transdermal bases such as Lipoderm, referred to as Phospholipid Base, for drug delivery across the skin. The purpose of this study is to characterize the percutaneous absorption of lorazepam 5 mg/g in Phospholipid Base, when applied to human cadaver torso skin, in vitro, using the Franz skin finite dose model.
Methods
The percutaneous absorption of lorazepam was evaluated using ex vivo human cadaver torso skin from 3 donors. The skin from each donor was cut into small sections to fit on nominal 2 cm2 Franz diffusion cells. A nominal volume equivalent to 5 mg formulation/cm2/skin section was then applied to a 2 cm2 dosing surface of 3 replicate skin sections for each donor. At predetermined time points (0, 2, 4, 8, 12, 24, 32, and 48 hr), the receptor solution within each chamber was removed, replaced with fresh receptor solution, and an aliquot of 6 mL was saved for analysis. Mean values for lorazepam total absorption, rate of absorption, skin content, and surface wash were quantified via HPLC analysis.
Results
Lorazepam mean total absorption was 8.38% ± 4.37, with a rise to peak rate of absorption at approximately 30 hr following dose application. Lorazepam was also found within the dermis and epidermis at 0.22% ± 0.02 and 3.65% ± 1.29 of the applied dose, respectively.
Conclusion
Results show that Phospholipid Base can facilitate the percutaneous absorption of lorazepam. This study’s findings may be helpful when justifying the viability of using Phospholipid Base as a vehicle for the transdermal delivery of lorazepam and could potentially be useful for practitioners and pharmacists considering the skin as an alternative route for the delivery of lorazepam.
Keywords: Lorazepam; Transdermal base; Transdermal delivery; Percutaneous absorption; Phospholipid Base; Pharmaceutical compounding; Franz skin finite dose model
Keywords |
|
| Lorazepam; Transdermal base; Transdermal delivery; Percutaneous absorption; Phospholipid Base; Pharmaceutical compounding; Franz skin finite dose model | |
Introduction |
|
| Lorazepam is an antianxiety agent used for the management of anxiety, insomnia, and chemotherapy-induced nausea and vomiting. Lorazepam belongs to a class of psychoactive drugs known as benzodiazepines [1]. The mechanism of action for lorazepam involves initial binding of the drug to benzodiazepine receptors within the Central Nervous System (CNS). The activated receptors allosterically interact with Gamma-Aminobutyric Acid (GABA) receptors, enhancing the effects of GABA, an inhibitory neurotransmitter. GABA then inhibits the arousal of various regions within the CNS, leading to CNS depression. As a result of the CNS depression, lorazepam is labeled as a sedative used in the treatment of anxiety and insomnia [2]. In addition, studies have shown that lorazepam, when combined with diphenhydramine, haloperidol, and/or metoclopramide, can be used off-label for the treatment of chemotherapy-induced nausea and vomiting [3,4]. | |
| Lorazepam can be administered via the oral, intramuscular (IM), or intravenous (IV) routes, all of which are conventional routes for medication administration [2]. Although oral administration of lorazepam is easy and convenient, this route is not suitable for all patients, such as those in hospice care due to swallowing difficulties. Similarly, though IM and IV administration of lorazepam have quick onset and are helpful in those with swallowing difficulties, these routes are invasive and painful, often leading to discomfort and noncompliance [5]. | |
| An ideal drug delivery system should be easy to administer and noninvasive to improve patient comfort and compliance [5]. Limitations associated with conventional routes of medication administration have led to the development of transdermal drug delivery systems. Transdermal delivery involves the application of medication onto the skin surface, which is intended to penetrate through the skin and into systemic circulation. This method of delivery is non-invasive, easy to administer, painless, and allows medications to bypass first pass metabolism [6]. However, not all drugs and formulations are suitable candidates for transdermal delivery. The skin is a natural barrier to drug absorption as it is the body’s first line of defense against toxins, pathogens, and other foreign materials [5]. The skin is composed of three layers: epidermis, dermis, and hypodermis. Within the epidermis, the stratum corneum is the outermost layer of the skin that serves as the main barrier to drug entry [7]. Penetration across the stratum corneum depends not only on the delivery vehicle, but also the physical and chemical properties of the drugs, such as: molecular weight, solubility, partition coefficient, and dissociation constant [6,7]. The ability of lorazepam transdermal formulations to penetrate into and through excised human skin under in vitro conditions was investigated by Puglia et al. The authors concluded that lorazepam, when combined with penetration enhancers (azone and propylene glycol) in a hydro-alcoholic gel formulation, was capable of penetrating the stratum corneum and epidermis of human skin [8]. | |
| Lorazepam transdermal formulations are not commercially available. Through pharmaceutical compounding, which involves the preparation of medications based on prescription orders to meet individual patient needs [9], lorazepam can be incorporated into transdermal bases such as Pluronic Lecithin Organo gel (PLO) or Lipoderm for transdermal delivery. PLO is a micro emulsion-based gel, while Lipoderm, also referred to as Phospholipid base, consists of a proprietary liposomal component shown to successfully facilitate the penetration of drugs into and through ex vivo human skin under in vitro conditions [10]. In 2008, two pilot trials conducted by Bleicher et al. showed that a transdermal formulation consisting of lorazepam, diphenhydramine, and haloperidol in PLO was efficacious for symptomatic control in patients with breakthrough chemotherapyinduced nausea and vomiting [3]. However, a study conducted by Smith et al. in 2012 using the same transdermal PLO formulation as that in Bleicher et al., showed that lorazepam serum levels were nondetectable at 240 min following application [11]. | |
| The percutaneous absorption of lorazepam, when in Phospholipid Base, has not yet been researched on human skin. The purpose of this study is to characterize the percutaneous absorption of lorazepam 5 mg/g in Phospholipid Base, when applied to human torso skin, in vitro, using the Franz skin finite dose model. This model utilizes the finite dose technique and Franz diffusion cells to dose and culture the skin samples. It has been shown to be a valuable tool in predicting in vivo percutaneous absorption kinetics of topically applied drugs [12]. | |
Materials and Methods |
|
| Skin preparation | |
| The percutaneous absorption of lorazepam was evaluated using ex vivo human cadaver torso skin from 3 donors without obvious signs of skin disease. The skin samples were dermatomed, cryopreserved, sealed in a water-impermeable plastic bag, and stored at approximately -70°C until the day of the experiment. Prior to use, skin samples were thawed in water at approximately 37°C and rinsed with tap water to remove blood or other material from the surface. The skin from each donor was then cut into small sections to fit on nominal 2 cm2 Franz diffusion cells, chambers specially designed to maintain the skin at a temperature and humidity that matches in vivo conditions. Within each chamber, the skin section was mounted on a diffusion apparatus so that the dermal layer is immersed in receptor solution while the epidermal surface is exposed to the ambient laboratory environment (humidity of 35% to 55% and temperature of 21°C ± 4) via the chimney. The receptor solution consisted of 0.1x-phosphate-buffered isotonic saline (13.7 mM NaCl, 0.27 mM KCl, 1 mM Na2HPO4, and 0.2 mM KH2PO4) pH (7.4 ± 0.1),0.1% Oleth-20, and 0.0084% Gentamicin, stirred magnetically at approximately 600 Revolutions per Minute (RPM) within the receptor compartment. Phosphatebuffered saline is often used within receptor solutions to mimic physiological conditions, maintaining skin viability and integrity. Gentamicin was added to prevent bacterial degradation of the drug, while Oleth-20 was used to improve solubility of the drug in receptor solution. The water jacket temperature was controlled to maintain skin surface temperature at 32.0°C ± 1.0. | |
| The integrity of the skin sections were assessed based on their permeability to Tritiated Water (3H2O) [13]. 3H2O forms when tritium, a radioactive form of hydrogen, binds to the oxygen atom [14]. Following a brief equilibrium period, approximately 500 μL of 3H2O (PerkinElmer, Boston, MA, sp. Act. ~ 0.5 μCi/mL) was layered across the entire skin surface using a repeater pipette. After 5 minutes, the 3H2O layer was removed and after 30 minutes, the receptor solution was collected and analyzed for radioactive content by liquid scintillation counting. This method quantifies radioactive content by detecting movement of the particles and converting it into electrical pulses that can be recorded [15]. Skin specimens with absorption of 3H2O less than 1.56 μL/cm2 were considered acceptable. Donor demographics and skin integrity results are shown in Table 1. | |
| Table 1: Donor demographics and skin integrity results. | |
| Preparation of test formula: lorazepam 5 mg/g in Phospholipid Base | |
| Lorazepam and the wetting agent propylene glycol 10% were first incorporated into the Phospholipid Base. The formulation was then mixed with an Electronic Mortar and Pestle (EMP) (Unguator® Technology, e/s model) for 3 minutes at a setting of 7, sheared twice using an ointment mill (Exakt Technologies, Inc., 50 model) (once at a setting of 2 and once at a setting of 1), and remixed with the EMP (1 minute at a setting of 5) to achieve content uniformity. Details relating to the test formula are shown in Table 2. Potency was confirmed through High-Performance Liquid Chromatography (HPLC) with a photo diode array detector. | |
| Table 2: Test formula: lorazepam 5 mg/g in Phospholipid Base. | |
| Dosing and sample collection | |
| Prior to dosing, receptor solutions were collected and the compartments were refilled with fresh receptor solutions. The chimney was next removed to allow for access to the epidermal surface for dose application. Using a calibrated positive displacement pipette, a nominal volume of approximately 7 mL (5 mg formulation/ cm2/skin section) was applied to the surface (2 cm2 dosing area) of three replicate skin sections for each donor, with a total of 9 skin sections for 3 donors. The dose of 10 mg/skin section was then evenly dispersed and rubbed onto the surface using a glass rod. Approximately five to ten minutes after application, the chimney was replaced. In order to assess for appearance of substances diffusing from the skin that may lead to cross-contamination or analytical interference, one skin section from each donor was left untreated to serve as control. At predetermined time points (0, 2, 4, 8, 12, 24, 32, and 48 hr), the receptor solution within each chamber was removed, replaced with fresh receptor solution, and an aliquot of 6 mL was saved for analysis. A total of 8 receptor samples were collected over 48 hours. After the last receptor sample was collected, each skin section was washed twice with 1 mL of 80:20 ethanol: water to remove unabsorbed formulation from the skin surface. Following surface wash, the skin was tape stripped up to 10 times to remove the stratum corneum, using 3M Transpore® surgical tape (manufactured by 3M, St. Paul, MN 55144), and extracted overnight in 3 mL of acetonitrile. The skin was then removed from the diffusion cell and separated into epidermis and dermis using scalpel and needle-point forceps, and extracted overnight at room temperature in 1 mL of 80:20 ethanol: water. Collected samples were stored within glass containers at approximately -20°C pending analysis. | |
| Sample analysis | |
| The quantification of lorazepam was by HPLC (Agilent Technologies, 1100 Series LC and LC/MS Systems). | |
| For analysis of receptor solution and stratum corneum extract, a gradient solvent system consisting of 0.1% formic acid in Distilled De-ionized Water (dd H2O) (solvent A) and methanol (solvent B) was run through a Zorbax Eclipse XDB- C18, 3.5μ (2.1× 50 mm) column at a flow rate of 0.4 mL/min. Diode array detector, set at 254nm, was used for solution comparison and solution stability. Eluting peaks were quantified using a mass spectrometer detector with a positive polarity with ions monitored at 321.10 m/z. For analysis of solution extracted from the surface wash, dermis, and epidermis, an isocratic solvent system consisting of 45% solvent A and 55% solvent B was used. The procedure and the equipment used for analysis were identical to that for receptor solution analysis. | |
Results |
|
| To characterize the percutaneous absorption of lorazepam, a total of 4 parameters were determined for each of the 9 chambers, as follows: total absorption, rate of absorption, skin content, and surface wash. Since each chamber had corresponding values for the 4 parameters, mean values and Standard Error (SE) were calculated for each parameter across the 3 donors. Mean values were also expressed as percentages of the applied dose. | |
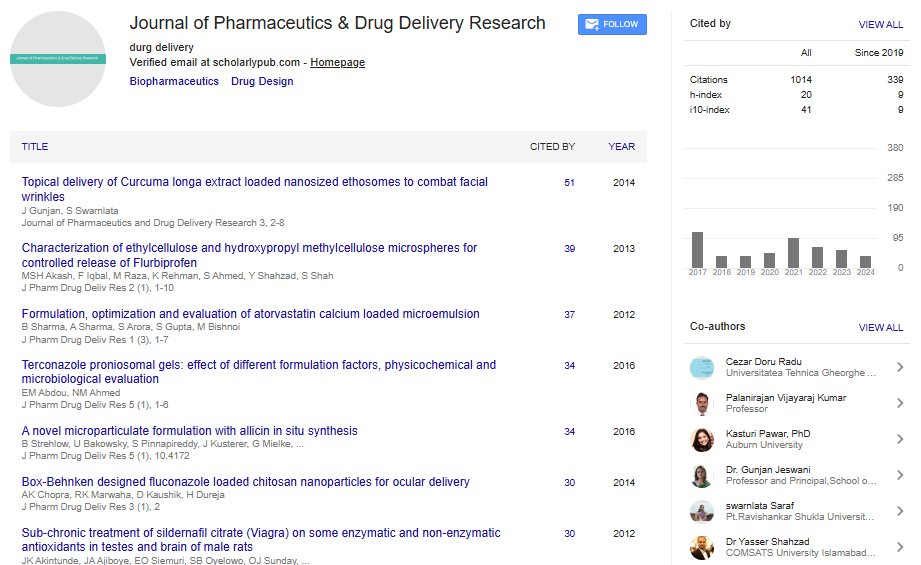
| Total absorption of lorazepam, defined as the mass of drug in receptor solution over 48 hours, was determined for each chamber. Mean total absorption (μg) was the average of total absorptions for all 9 chambers from the 3 donors. The mean total absorption (μg) of lorazepam, when in Phospholipid Base, was 4.54 μg ± 2.36, corresponding to 8.38% ± 4.37 absorption of the applied dose (Table 3, Figure 1). | |
| Table 3: Distribution of lorazepam into and through ex vivo human torso skin over 48 hr from a single application. Mean ± SE, n=3 donors, as mass recovered (�?µg) and percent of applied dose (%). | |
| Figure 1: Permeation of lorazepam and distribution within the skin layers 48 hr after application. Results are expressed as mean ± SE. | |
| Rate of absorption, presented as flux (μg/cm2/hr) of lorazepam into receptor solution, was determined by dividing the amount of lorazepam absorbed during a time interval and the length of that interval. Flux is not a discrete and directly measurable value. Rather it is a time-averaged value reported at midpoint of sample collection for a sampling period. For instance, if samples are collected at 4 and 8 hr, the flux of lorazepam during that time interval is equal to the amount of lorazepam in the receptor solution between 4 and 8 hr, divided by the time span of 4 hr. Flux is then plotted at 6 hr, midpoint of 4 and 8 hr. Mean flux (μg/cm2/hr), was calculated across donors for each sampling interval at midpoint, as displayed in Table 4 and Figure 2. Using the mean flux data at midpoint, an actual mean flux for the whole study (over 48 hr) was calculated and estimated to be 0.047 μg/cm2/hr. Mean cumulative amount of drug absorbed (μg/cm2) into receptor solution at predetermined time points (Table 5, Figure 3) were estimated using mean flux results. A cumulative amount of 2.278 μg/cm2 of lorazepam was detected at 48 hr, which is equivalent to a total of 4.566 μg for a 2 cm2 dosing area, a value that is comparable to that obtained from direct HPLC analysis of the receptor solution (total absorption). | |
| Figure 2: Across donor summary: mean flux (�?µg/cm2/hr) ± SE for lorazepam 5 mg/g in Phospholipid Base. | |
| Figure 3: Estimated cumulative amount of lorazepam (�?µg/cm2) absorbed over time. | |
| Table 4: Across donor summary (n=3 donors): mean flux (�?µg/cm2/hr) ± SE at midpoint. | |
| Table 5: Estimated mean cumulative amount absorbed (�?µg/cm2) at predetermined time points. | |
| Skin content (μg) refers to the amount of lorazepam found within the stratum corneum, dermis, and epidermis after 48 hr. Mean skin content was calculated as the average lorazepam content in the stratum corneum, dermis and epidermis from the 9 skin sections across 3 donors, as displayed in Table 3, Figure 1. Mean lorazepam skin content was 2.25 μg ± 0.84 for the stratum corneum,0.12 μg ± 0.01 for the dermis, and 1.99 μg ± 0.70 for the epidermis, corresponding to 4.13 % ± 1.53, 0.22 % ± 0.02, and 3.65% ± 1.29 of the applied dose, respectively. The mean percentage of applied dose found within the receptor solution (total absorption), dermis, and epidermis were then summed to obtain a mean of 12.25% permeation of the applied dose through the stratum corneum. Surface wash (μg) is to the amount of lorazepam remaining on the surface of the skin after 48 hours of dose application. Mean lorazepam content within surface wash was 45.10 μg ± 1.92, corresponding to 83.06 % ± 3.73 of the applied dose (Table 3). The mean percentages of applied dose found in receptor solution, dermis, epidermis, stratum corneum, and surface wash were summed to obtain a total recovery of 99.44 % ± 2.80 of the applied dose, as displayed in Figure 1. | |
Discussion |
|
| Phospholipid Base is widely used in pharmaceutical compounding for drug delivery across the skin [16]. Results of this study show that the Phospholipid Base was capable of facilitating the percutaneous absorption of lorazepam across ex vivo human cadaver torso skin using the Franz skin finite dose model. As previously discussed, this model has shown to be a valuable tool used in the prediction of in vivo percutaneous absorption of topically applied drugs [12]. When lorazepam 5 mg/g in Phospholipid Base was applied to skin surfaces, lorazepam was absorbed through the skin layers, into the receptor solutions. The estimated cumulative amount of lorazepam that permeated the 2 cm2 skin surface using mean flux results was equivalent to the value obtained for mean total absorption after 48 hr. Lorazepam was also found in the stratum corneum, dermis, and epidermis, which show that this drug has the ability to penetrate into and through the skin, when in Phospholipid base. The stratum corneum is a major barrier to drug delivery and not all drugs and formulations are suitable candidates for delivery through the skin [5]. Despite the large amount of lorazepam being recovered from the surface wash, lorazepam was able penetrate the skin, with a slow and steady rate of absorption, as displayed in Figure 2. There was a rise in flux to peak at approximately 30 hr following dose application. Though the large SE associated with mean flux results is a limitation for this study, this could potentially be prevented in future studies by increasing sample size. | |
| Lorazepam is commercially available in various dosage forms. Lorazepam tablets USP (TEVA Pharmaceutical Industries Ltd.) and lorazepam oral concentrate USP (Hi-Tech Pharmacal Co., Inc.) have an absolute bioavailability of 90% [17,18], while Ativan (lorazepam) injection USP (West-Ward Pharmaceuticals) has a bioavailability of 100% when administered via IV and IM routes [19]. When comparing lorazepam bioavailability via these conventional routes (e.g. oral, IV, IM) to results of this study, a 12.25% penetration of the applied dose through the stratum corneum and 8.38% of the applied dose in receptor solution following transdermal application of lorazepam 5 mg/g in Phospholipid Base are minute amounts. However, the Phospholipid Base formulation was applied to torso skin, which is known to be thicker and more difficult to penetrate than skin in areas such as the inner wrists that are traditionally targeted for delivery of medication through the skin [20,21]. Therefore, it is expected that application of the transdermal formulation to torso skin may underestimate the delivery of the drug in comparison to if it were to be applied to skin on other parts of the body. In addition, the dosing surface was limited to 2 cm2. Increasing the size of the dosing area could potentially improve total drug absorption. | |
| While results show that Phospholipid Base is an appropriate vehicle for the transport of lorazepam across human skin, since the study was conducted in vitro, results cannot be extrapolated to conclude that lorazepam therapeutic blood levels will be achieved following a single application of the lorazepam formulation. For instance, in Bleicher et al. though results showed that the lorazepam, diphenhydramine, and haloperidol in PLO formulation was efficacious for symptomatic control in patients with breakthrough chemotherapy-induced nausea and vomiting [3], Smith et al. later showed that lorazepam serum levels were non-detectable following application of the same transdermal PLO formulation [11]. Given the contradicting scientific evidence for PLO, it may be necessary that further studies be conducted in vivo to assess the ability of other bases such as Phospholipid Base to deliver lorazepam through human skin. In addition, considering the sparse scientific evidence relating to transdermal delivery of lorazepam, having data to show that lorazepam, when in Phospholipid Base, is able to penetrate excised human skin could potentially be helpful when justifying the viability of percutaneous delivery of this drug, which may be necessary when conventional routes of administration are not viable for certain patients due to clinical or functional reasons. Having an alternative route of administration for lorazepam using Phospholipid Base may also allow practitioners and pharmacists to customize each patient’s medication regimen. This study’s results may also be a stepping stone for designing future studies and predicting in vivo percutaneous absorption of lorazepam. For instance, in an in vitro study conducted by Puglia et al., researchers discovered that a lorazepam formulation containing penetration enhancers, when applied to excised human skin, was able to penetrate the stratum corneum and epidermis. Using flux values from that study, researchers were then able to predict in vivo lorazepam steady state plasma concentrations [8]. However, such prediction is only theoretical and future in vivo studies are needed to establish such in vitro in vivo correlation. | |
Conclusion |
|
| When evaluating the total absorption, rate of absorption, and skin content of lorazepam 5 mg/g in Phospholipid Base using the Franz skin finite dose model, results of this study show that the Phospholipid Base was capable of facilitating the percutaneous absorption of lorazepam into and through excised human torso skin in vitro. Knowledge of this study’s results could potentially be useful for practitioners and pharmacists considering the skin as an alternative route for the delivery of lorazepam in patients with anxiety, insomnia, or chemotherapy-induced nausea and vomiting. The study’s findings may also be helpful when justifying the viability of using Phospholipid Base as a vehicle for the transdermal delivery of lorazepam. | |
Acknowledgments |
|
| The authors would like to thank Paul A. Lehman, M Sc (Cetero Research, Fargo, ND, USA) for conducting the Franz skin finite dose model experiments. | |
Authors��? contributions |
|
| All authors have substantially contributed to this manuscript and meet the criteria for authorship. | |
Conflicts of interest |
|
| The authors are employed by Professional Compounding Centers of America (PCCA), the manufacturer of the Phospholipid Base discussed in the manuscript. | |
References |
|
|
|
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi