About the Journal of Liver: Disease & Transplantation

Journal of Liver: Disease & Transplantation (JLDT) is a peer-reviewed scholarly journal which aims to publish the most complete and reliable source of information on the discoveries and current developments in the mode of original articles, review articles, case reports, short communications, etc. in all areas of liver pathology and making them available online.
The following classifications and topics related to liver will be considered for publication in the Journal of Liver: Disease & Transplantation but, not limited to the following fields:
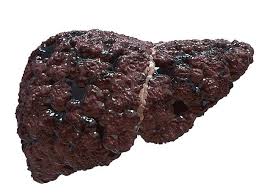
- Liver Failure
- Chronic Hepatitis
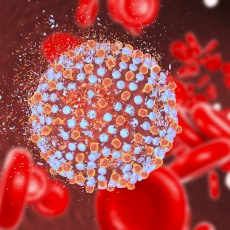
- Viral Hepatitis
- Liver Complications
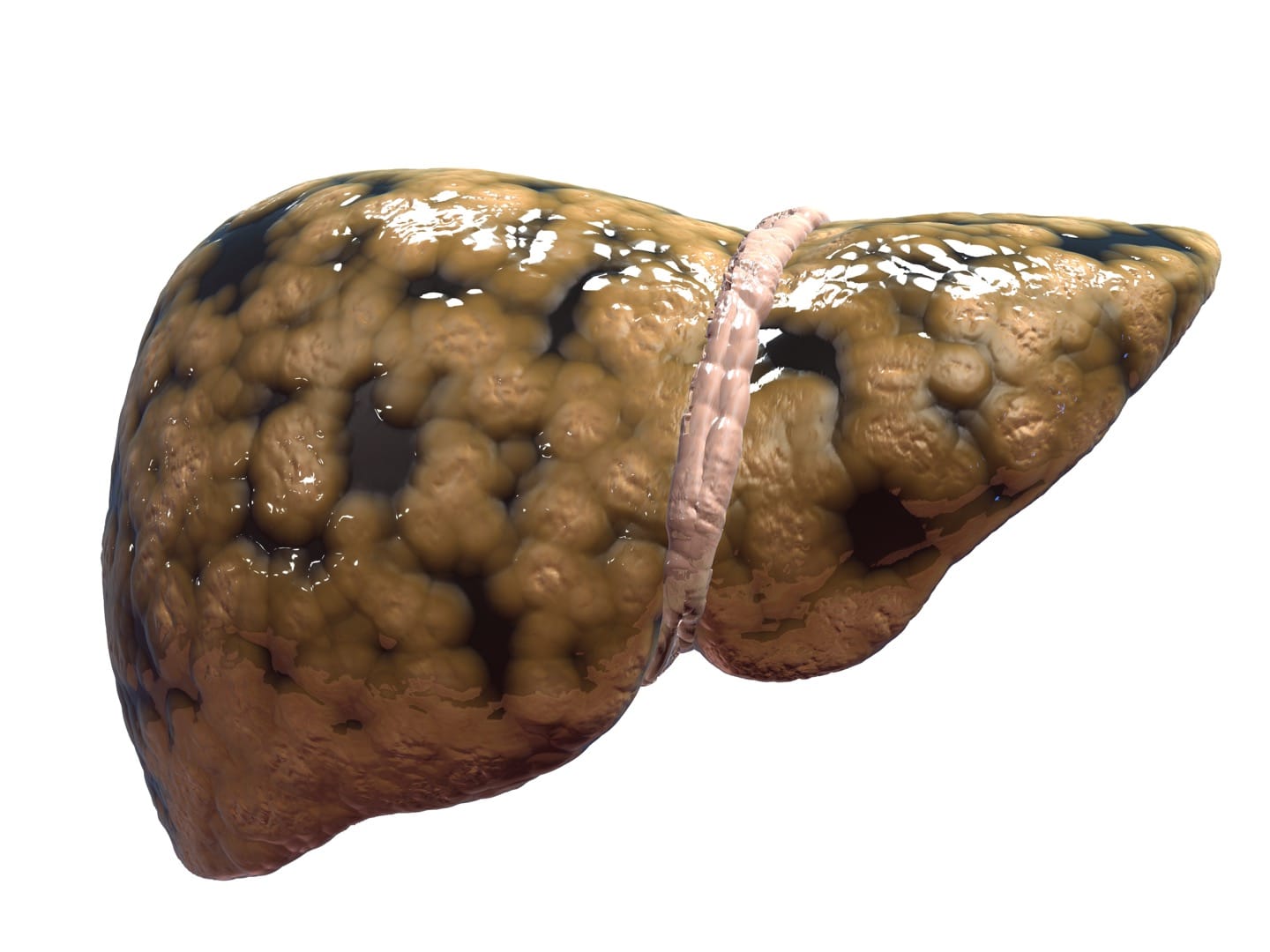
- Liver Cirrhosis
- Liver Physiology
- Liver Pathology
- Fatty Liver
- Gastrointestinal Disorders
- Liver Genetics
- Autoimmune Liver Diseases
- Liver Immunology
- Liver Transplantation
- Transplantation Outcomes
- Post transplantaion Care
Any other material of Liver Diseases and Liver Transplantation relevance will also be considered.
The Journal uses Editorial Tracking System for quality in review process. Editorial Tracking is an online manuscript submission, review and tracking system. Review processing is performed by the editorial board members of Journal of Liver: Disease & Transplantation or outside experts; at least two independent reviewers approval followed by editor approval is required for acceptance of any citable manuscript. Authors may submit manuscripts and track their progress through the system, hopefully to publication. Reviewers can download manuscripts and submit their opinions to the editor. Editors can manage the whole submission/review/revise/publish process.
Interested authors are encouraged to submit manuscripts through Online Submission System or send as an e-mail attachment to the Editorial Office at editorialoffice@scitechnol.com
Liver Biology
Liver is the glandular organ that stores and metabolizes nutrients, detoxifies, and produces bile salts. Liver is the largest organ of human body. The study of anatomy and functions of the liver is known as Liver Biology.
Liver Physiology
The study of functions and activitiesof the liver is known as Liver Physiology. It also dealswith the way in which the Liver and its parts function
Liver Functions
Functions of the liver include:
Production of Bile, which helps carry away waste and break down fats in the small intestine during digestion,
Production of proteins for blood plasma and detoxification of blood.
Liver Pathology
The study of Liver diseases is called Liver pathology. Liver diseases can be inherited or caused by a variety of factors that damage the liver, such as viruses and alcohol use. Liver diseases include the following conditions: Cirrhosis, Inflammation or hepatitis.
Hepatology
Hepatology is the branch of medicine that incorporates the study, prevention and diagnosis of liver, gallbladder, biliary tree, and pancreas as well as management of their disorders but is not limited to, the study of acute and chronic hepatitis, viral hepatitis, genetic and metabolic liver diseases and their complications.
Liver Disease Diagnosis
Liver disease can often be difficult to diagnose because its symptoms can be vague and easily confused with other health problems. Blood tests can look for the presence of liver inflammation or screen for antibodies or virus particles that might indicate a specific form of liver Disease. These tests are called Liver Tests.
Translational Hepatology
The fundamental concept underlying the Translational Hepatology is that human disease can serve as a window into broad biological processes, the understanding of which could, in turn, lead to treatments for these and other diseases.
Immunology of Hepatobiliary systems
The hepatobiliary system is essential for digestion and includes: the liver, pancreas, bile ducts and the gallbladder. Many disorders and diseases can affect these organs of hepatobiliary system. Immunology deals with the defence mechanisms including all physical, chemical and biological properties of the organism that help it to combat its susceptibility to foreign organisms, material, etc.
Gastrointestinal Disorders
The medical specialty devoted to the study, diagnosis and treatment of disorders of the digestive system. These disorders may affect the esophagus (swallowing tube), stomach, small intestine, large intestine (colon), rectum, liver, gallbladder, or pancreas.
Transplantation Biology
The science of transferring a graft from one part of the body to another or from one individual to another is known as Transplantation. The graft may consist of an organ, tissue, or cells. If donor and recipient are the same individual, the graft is autologous. If donor and recipient are genetically identical it is syngeneic. If donor and recipient are any other same-species individuals, the graft is allogeneic. If the donor and recipient are of different species, it is called xenogeneic.
Transplantation Complications
Complications of a liver transplant can include rejection, an increased risk of infection, graft failure, biliary conditions and a higher risk of developing certain conditions – including some types of cancer.
Transplantation & Immunosuppressive Management
Immunosuppression involves an act that reduces the activation or efficacy of the immune system. Some portions of the immune system itself have immunosuppressive effects on other parts of the immune system, and immunosuppression may occur as an adverse reaction to treatment of other conditions.
Posttransplantation Care
After liver transplantation care must be taken because the complications don’t arise soon after the transplantation. They may arise after 2 or 3 weeks. Hence patients must be shifted to ICU and must be under observation. This is known as Post Transplantation care.
Digestive Disorders
Digestive disorder is any health problems that occurs in the digestive tract. Some common problems include Heart burn/GERD, Irritable bowel syndrome and Lactose intolerence. Symptoms may include Bloating, diarrhoea, gas, stomach pain and stomach cramps.
Liver Cancers
It is also known as Hepatic Cancer, which starts in the liver. It is a condition that happens when normal cells in the liver become abnormal and grow out of control into cáncer.
Liver Hepatitis
Hepatitis is swelling and inflammation of liver. Hepatitis is most commonly caused by viral infection. Other causes of Hepatitis include autoinmune hepatitis (a disease occuring when the body makes antibodies against the liver tissue) and hapatitis that occurs as a secondary result of medications, drugs, toxins and alcohol.
Liver Cirrhosis
Cirrhosis is a slowly progressing Disease in which healthy liver tissue is replaced with scar tissue, eventually preventing liver from functioning properly. The scar tissue blocks the flow of blood through the liver and slows the processing of nutrients, hormones, drugs and naturally produced toxins.
Liver Failure
Liver failure is a life threatening condition that demands urgent medical care. Most often, liver failure occurs gradually and over many years. Rare condition known as acute liver failure occurs rapidly within 48hrs and difficult to detect initially.
Liver Regeneration
The liver has a remarkable capacity to regenerate after injury and to adjust its size to match its host. Within a week after partial hepatectomy, which, in typical experimental settings entails surgical removal of two-thirds of the liver, hepatic mass is back essentially to what it was prior to surgery.
Liver Disease Complications
These include high blood pressure in the veins that supply the liver, swelling inthe legs and abdomen, enlargement of spleen, bleeding, infections, malnutrition, jaundice, bone diseases, increased risk of liver cáncer and acute-or-chronic cirrosis.
Fast Editorial Execution and Review Process (FEE-Review Process):
Journal of Liver: Disease & Transplantation is participating in the Fast Editorial Execution and Review Process (FEE-Review Process) with an additional prepayment of $99 apart from the regular article processing fee. Fast Editorial Execution and Review Process is a special service for the article that enables it to get a faster response in the pre-review stage from the handling editor as well as a review from the reviewer. An author can get a faster response of pre-review maximum in 3 days since submission, and a review process by the reviewer maximum in 5 days, followed by revision/publication in 2 days. If the article gets notified for revision by the handling editor, then it will take another 5 days for external review by the previous reviewer or alternative reviewer.
Acceptance of manuscripts is driven entirely by handling editorial team considerations and independent peer-review, ensuring the highest standards are maintained no matter the route to regular peer-reviewed publication or a fast editorial review process. The handling editor and the article contributor are responsible for adhering to scientific standards. The article FEE-Review process of $99 will not be refunded even if the article is rejected or withdrawn for publication.
The corresponding author or institution/organization is responsible for making the manuscript FEE-Review Process payment. The additional FEE-Review Process payment covers the fast review processing and quick editorial decisions, and regular article publication covers the preparation in various formats for online publication, securing full-text inclusion in a number of permanent archives like HTML, XML, and PDF, and feeding to different indexing agencies.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi