Editorial, Cell Biol Res Ther Vol: 1 Issue: 1
Inflammation and Pancreatic Cancer: A Tale of Two Cytokines
| Wei Li1, Andrew M. Albrecht2, and Min Li2* | |
| 1College of Medicine, Shandong University of Traditional Chinese Medicine, Jinan, Shandong 250355, China | |
| 2The Vivian L. Smith Department of Neurosurgery, The University of Texas Medical School at Houston, Houston, Texas 77030, USA | |
| Corresponding author : Min Li, PhD The Vivian L. Simith Department of Neurosurgery, The University of Texas Medical School at Houston, 6431 Fannin Street, MSE R266, Houston, TX, 77030, USA Tel: (713) 500-6491 Fax: (713) 500-6493 E-mail: Min.Li@uth.tmc.edu |
|
| Received: June 22, 2012 Accepted: June 22, 2012 Published: June 25, 2012 | |
| Citation: Li W, Albrecht AM, Li M (2012) Inflammation and Pancreatic Cancer: A Tale of Two Cytokines. Cell Biol: Res Ther 1:1. doi:10.4172/2324-9293.1000e104 |
Abstract
Inflammation and Pancreatic Cancer: A Tale of Two Cytokines
Pancreatic cancer is the most fatal of all gastrointestinal (GI) cancers, with only a 5.8% survival rate beyond five years after initial diagnosis. This cancer is characterized by a high mortality, rapid progression, and resistance to chemo and radiation therapy. Surgical resection is the only curative treatment for pancreatic cancer, but only less than 15% patients are eligible for surgery. The front-line treatment for metastatic pancreatic cancer has been adjuvant chemotherapy trials of gemcitabine and gemcitabine-based combinational therapy. However, over the past decade, no significant advances in efficacy of chemotherapeutic treatment have arisen, and the mean survival rate of those who have undergone such treatment has not improved.
| Pancreatic cancer is the most fatal of all gastrointestinal (GI) cancers, with only a 5.8% survival rate beyond five years after initial diagnosis. This cancer is characterized by a high mortality, rapid progression, and resistance to chemo and radiation therapy. Surgical resection is the only curative treatment for pancreatic cancer, but only less than 15% patients are eligible for surgery. The front-line treatment for metastatic pancreatic cancer has been adjuvant chemotherapy trials of gemcitabine and gemcitabine-based combinational therapy. However, over the past decade, no significant advances in efficacy of chemotherapeutic treatment have arisen, and the mean survival rate of those who have undergone such treatment has not improved [1]. The rise in chemo-resistant pancreatic cancer has led to an urgent need for an alternative treatment. A full understanding of the biology and mechanisms underlying this disease will significantly improve our methods of treatment and drug design. Research into these mechanistic studies has led to a growing area of interest in the role of cytokines in pancreatic cancer progression, in particular the creation of a favorable tumorigenic conditions and aggressively resistant metastasis [2]. Studies have demonstrated their ubiquity in all stages of cancer development, but the question remains: can such a functionally pleotropic and chemically diverse class of molecules be targeted for treatment of pancreatic cancer? This review summarizes our current understanding of the role cytokines play in pancreatic cancer's resilience and its resistance to treatment focusing on two major pro-inflammatory cytokines, its role in tumor microenvironment necessary for growth and metastasis, and their potential for therapeutic and diagnostic procedures. |
| Cytokines are a vast and diverse group of glycosylated peptides produced by virtually all nucleated cells in human body, and play important roles in regulating cell growth, inflammation, and tumor metastasis. One of the characterizing features of pancreatic cancer is its rapid and aggressive metastatic behavior, and research into the pathways behind this action strongly implicates the involvement of overexpression of pro-inflammatory cytokines such as interleukin-6 (IL-6) and interleukin-8 (IL-8) [3]. These pro-inflammatory cytokines play a critical role in the activation of signal pathways controlling aggressive cell growth such as angiogenesis pathway though the action of vascular endothelial growth factor (VEGF), a cytokine which enhances angiogenesis and facilitates metastasis [2]. Targeting those pro-inflammatory cytokines may represent a new strategy for interventional molecular therapy. IL-6 has been shown to be overexpressed in human pancreatic cancer cells, and exogenous IL-6 increased the secretion of multiple Th2 type of cytokines. IL-6 also activated extracellular signal-regulated kinase2 (ERK2) signaling pathways in pancreatic cancer cells, indicating that IL-6 may be involved in promoting human pancreatic cancer development by furnishing Th2 type of cytokine environment and upregulating cell proliferation and angiogenesis related genes [4]. Recent study has shown that IL-8 was upregulated under the hypoxic conditions which mimics the human disease. IL-8 upregulated the expression of VEGF and activated ERK1/2 signaling pathway in pancreatic cancer cells. These data suggest that IL-8 might be a malignant factor in human pancreatic cancer and targeting IL-8 along with other anti-angiogenesis therapy could be an effective treatment for this malignancy [5]. These two cytokines therefore represent a major focus of current oncogenic cytokine research, as they play a large part in the deadly behavior of pancreatic tumors. |
| The resistance of pancreatic cancer to chemotherapy is a major challenge, partially due to the presence of fibroblastic stroma, which in essence blocks the majority of chemotherapeutic drugs from perfusing to the tumor [3]. Furthermore, pancreatic cancer's high mortality rate resides primarily in its highly efficient and aggressive metastasis owing to a favorable microenvironment suitable for tumor growth. Complicating the issue of cytokines' role in pancreatic cancer progression is the fact that they act in a paracrine signaling manner to communicate and coordinate with their non-cancerous cellular surroundings to create local hypoxia associated with pancreatic tumors. Chronic inflammatory diseases have become the focus of much of the research in cancer prevention, as it is now known that cytokines play a role in inflammation as well as acting to promote cancer progression, metastasis, and malignant transformation [6]. IL-8 is heavily associated with chronic pancreatitis, a condition which increases the likelihood of pancreatic cancer occurrence by a factor of 20 or more due to the convergence of inflammatory mediators and cytokines onto a common pathway [7]. Thus, IL-8 is activated by inflammation, which then acts through a positive paracrine feedback loop via up-regulation of several inflammatory mediators to maintain inflammation and promote angiogenesis [8]. The ability of IL-6 to enhance the secretion of pro-inflammatory cytokines typically seen expressed in Th2 lymphocytes also demonstrated that it plays a similarly important role in the inflammatory process as well [4]. The current aim is to use targeted molecular therapy to inhibit the oncogenic ability of pancreatic cancer cells by inhibiting this common pathway. The trouble with this approach is the complicated communication between the tumor cells and the stromal fibroblasts as well as immune effectors. For instance, IL-8 is known to bind to multiple receptors, and it appears that other than hypoxia, a variety of molecules can induce IL-8 including NO, oxidative stress, and acidosis, while both IL-8 and IL-6 are inducible through action of TNF-a [2]. Therefore, further elucidation of the entirety of the wide spectrum of chemical cross-talk involved in establishing tumor microenvironment may be a promising avenue for future therapy [9]. |
| The current strategy is to focus on eliminating inflammation and metastatic growth by targeted molecular therapy combined with early detection using predictive diagnostic cytokine tumor markers [10,11]. However, predictive, diagnostic, or prognostic use of tumorassociated cytokines has not been fully understood. The most reliable predictor of patient performance, IL-6, is at best prognostic of about half of those with pancreatic cancer [2]. However, this method is 100% predictive of a less than 1 year survival in those who have an IL-6 level greater than 5.2 pg/ml [2]. Research into pancreatitis has demonstrated a prognostic link between IL-6, IL-8, and TNF-a and the severity of acute pancreatitis, illustrating a potential in establishing a link between these inflammatory cytokines as indicators of tumor severity [10]. Likewise, the use of molecular targeted therapy is still in its infancy in pancreatic cancer. Several studies have demonstrated that selective blocking of IL-8 secretion by targeting specific integrins has shown significant inhibition of metastasis but has not shown complete abolishment of tumor growth [2,9]. Similar studies have suggested the therapeutic targeting of cytokines which are directly involved in establishing the tumor microenvironment, such as STAT3, an essential convergence point for multiple cytokine pathways [12]. Research has indicated that the complex interaction of cytokines with pancreatic cancer cell-signaling pathways and the multitude of chemical cross-talk occurring between microenvironment and tumor make it unlikely that any single molecular target will be effective. Rather, the most effective treatment will be one that involves a combination of multiple targeted molecular therapies as well as the implementation of earlier diagnostics utilizing correlative chemokine tumor markers. For instance, previous studies have shown a direct correlation between IL-8 levels and tumor growth and angiogenic potential. An increased level of IL-8 production is in part directly responsible for oncogenic activity and the aggressive metastasis seen in pancreatic tumors [13]. Those results indicate that IL-8 plays a critical role in tumorigenicity and may be used as a starting point for future development of earlier diagnostic techniques using IL-8 as an indicator of early-stage pancreatic cancer. Cytokines are an incredibly complex field of interacting molecular signals, further clouded by the fact that cytokines often aid in the regulation of other cytokines and growth factors in multiple signal cascades. It has been shown that both IL-6 and IL-8 can upregulate VEGF and activate the angiogenesis pathway, and are secreted in response to local hypoxia [8]. We have also found that a cancer master switch gene ZIP4 activates IL-6/ STAT3 pathway through a zinc dependent transcription factor CREB, which increases the pancreatic cancer cell growth [14]. Thus, as we begin to connect the pathways and form a more fundamental understanding of the mechanisms behind pancreatic cancer's deadly behavior, a wealth of potential targets and novel avenues of therapy will become available in order to combat this devastating disease. |
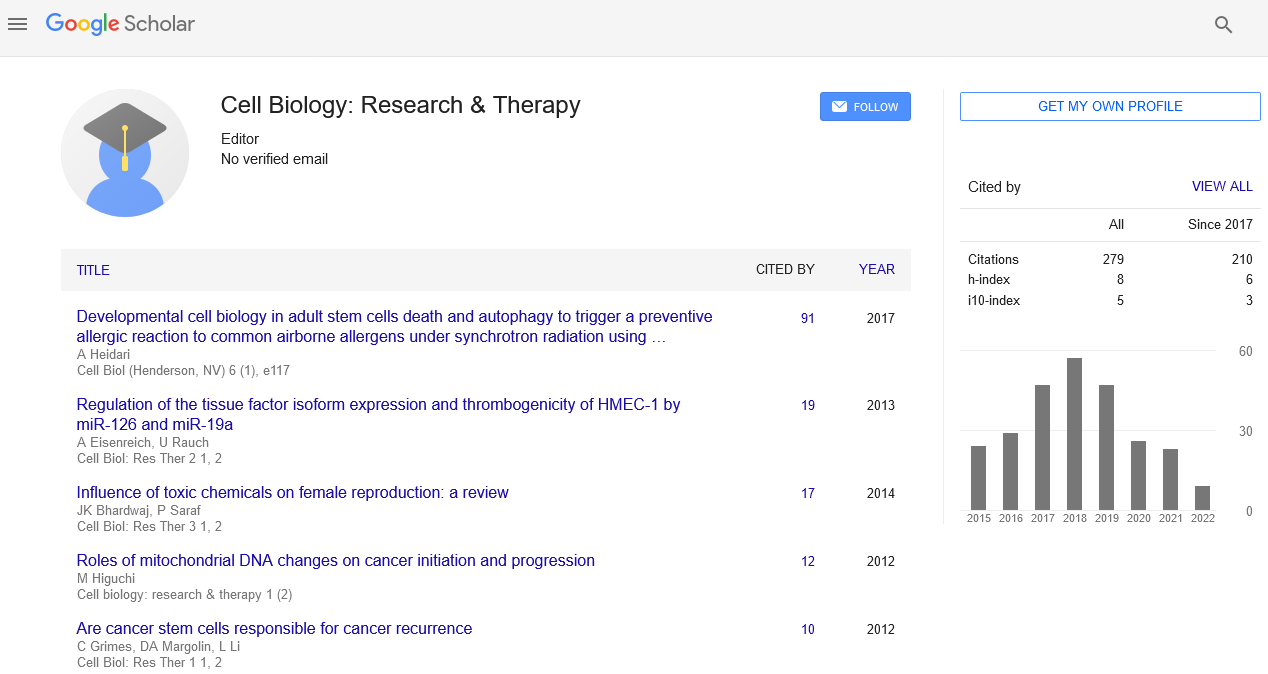
| While much is still to learn about the role of cytokines in pancreatic cancer, a promising future of combinational targeted molecular therapy is certainly on the horizon. Cell Biology: Research & Therapy (CBRT) provides the most immediate, relevant, and accurate information regarding basic cell biology, translational research, and novel diagnostic and therapeutic strategies relating to vital molecular disease processes, mechanisms, and interactions. Published by SciTechnol, this journal is backed by a multinational editorial board of highly qualified researchers, ensuring an accurate and quality peer review process and publication. Utilizing electronic resources and online content, the CBRT reflects a standard of quality of content and ease of timely publication. |
| There has been considerable progress made in the study of viruses and how they infect, replicate and spread inside hosts and host cells. Much is known about how viruses change their genome and proteins throughout their life cycles. However, our understanding of how the host cell itself changes during the virus life cycle is less well developed. Both genomic and proteomic changes are expected to occur during virus propagation, and genomic analyses of the cellular 'transcriptome' have been especially fruitful during the past decade. However, our understanding of host protein responses is even more poorly developed. These –omic responses can reflect particular host metabolic pathways, such as immunological strategies, that are activated in response to the infecting virus. These genomic and proteomic changes also may suggest ways in which the infecting virus alters the cell components to aid its propagation. By studying not only how the virus changes during infection, but how the host responds, one might determine which of these responses are important for viral survival, and exploit them for antiviral purposes. |
References |
|
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi